If you’re trying to understand IV therapy components—whether you’re studying medicine, working in healthcare, or just want to know what’s happening when you get an IV—you’ve come to the right place. We get it: looking at all those tubes, bags, and medical devices can feel overwhelming, especially when your health or job depends on getting it right. This guide breaks down every piece of IV equipment in a way that actually makes sense.
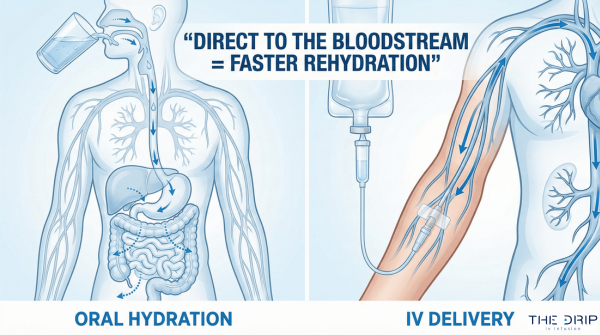
An intravenous (IV) system is basically a medical setup that gets fluids, medications, and nutrients straight into your bloodstream through a bunch of connected parts including IV tubing, catheters, drip chambers, injection ports, roller clamps, filters, connectors, and IV bags that all work together to make sure your treatment is safe and accurate.
Here’s What You Need to Know:
- IV tubing is like the highway that carries fluids from the bag to your body, made from materials like standard PVC or DEHP-free alternatives that meet ISO 8536-4:2019 safety standards
- IV catheters come in six standard sizes (14G-24G) with flow speeds from 20-240 mL/min, using materials like polyurethane that actually get softer after they’re put in
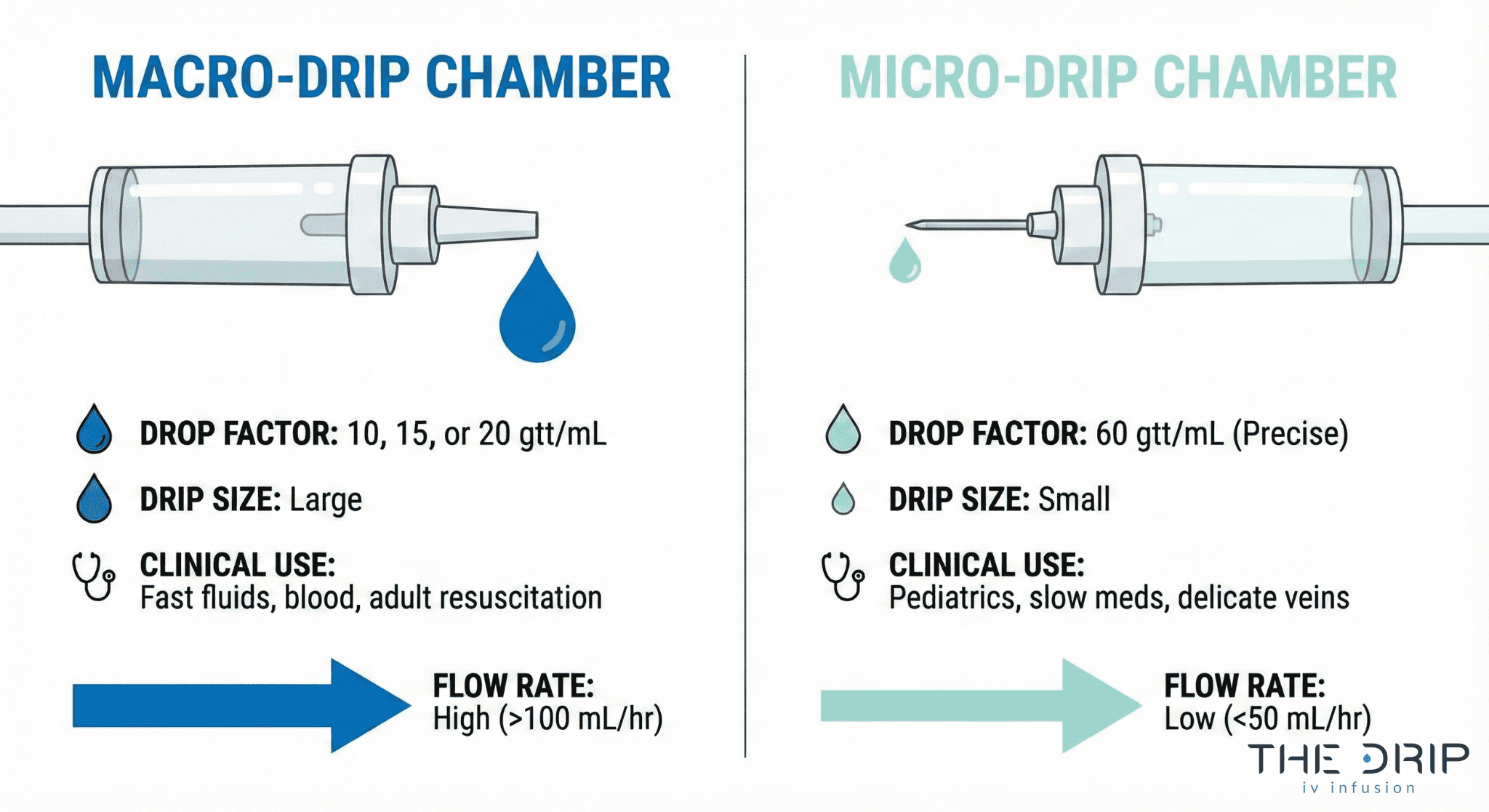
- Drip chambers stop air from getting into your blood while controlling flow through big-drip (10-20 drops/mL) or tiny-drip (60 drops/mL) setups
- Injection ports let nurses give you medicine without sticking you again, using needle-free connectors with germ-fighting coatings
- Roller clamps control how fast your IV flows by hand, though electronic versions work much better
- IV filters clean out bad stuff using 0.22-micron screens for bacteria or 1.2-micron filters for fatty solutions
- Connectors and extension sets use Luer-lock mechanisms to keep everything locked tight and reduce the chance things come apart
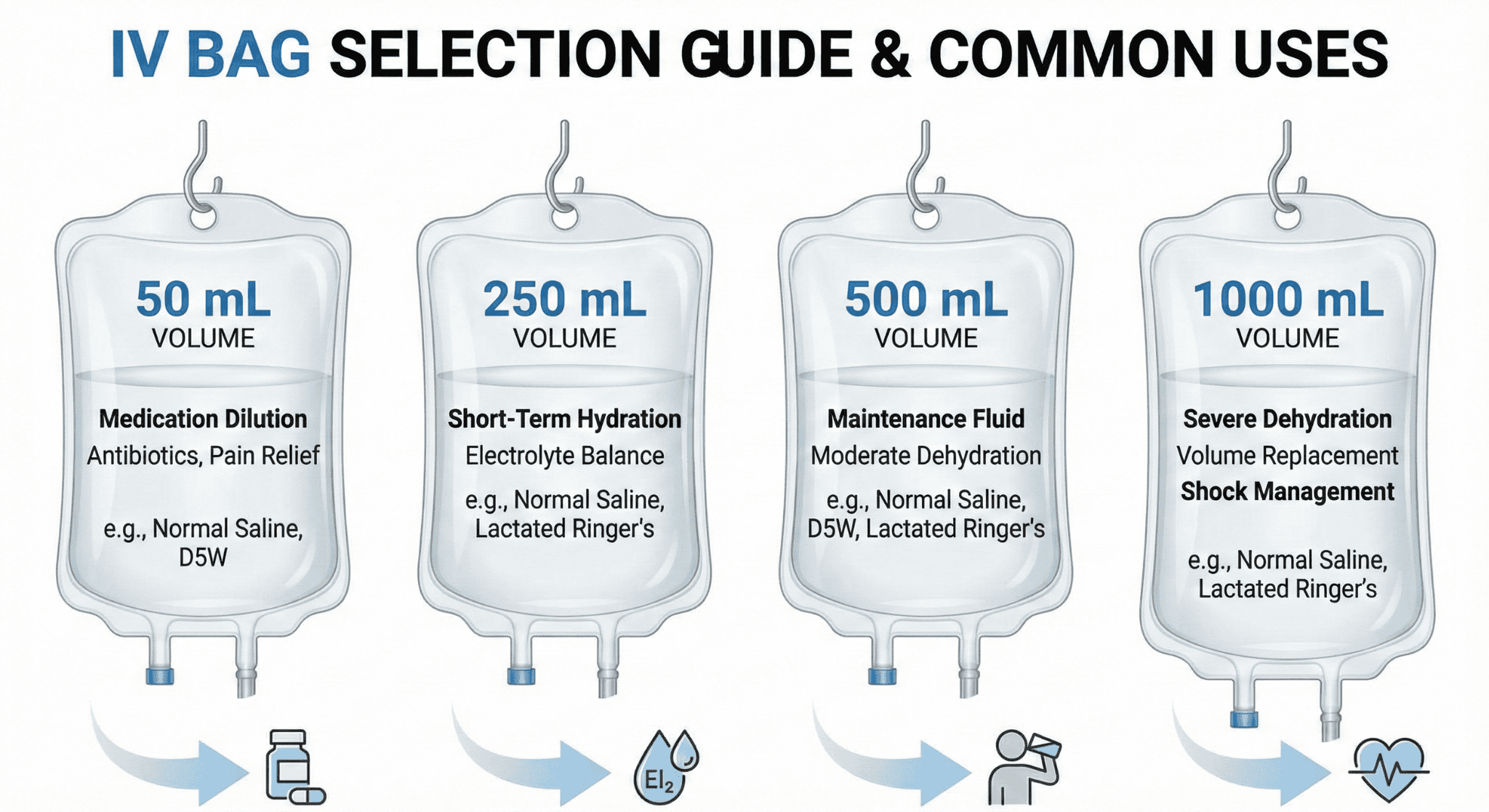
- IV bags hold different fluids in 50-1000 mL sizes, with non-PVC options that avoid chemical problems
- Problems happen with 35-50% of peripheral IVs, including fluid leaking out (17.8%), blockages (10.8%), and vein irritation (10.5%)
- Having medical professionals oversee everything makes sure the right parts get chosen and used safely
Pro Tip: When you’re looking at IV components, always check for FDA approval markings and make sure all the pieces work together—mismatched parts can mess up flow rates and put patients at risk.
What Is IV Tubing and Why Is It Essential in IV Therapy?
IV tubing is the flexible medical tube that connects an IV fluid bag to the catheter in your vein, letting controlled amounts of fluids and medications flow into your body. Think of IV tubing as the main pipeline that carries everything from the source to your bloodstream at just the right speed.
The tubing system has main lines for continuous drips and side lines for medicines given now and then. Modern IV tubing has multiple safety features built right in, like injection ports, drip chambers, and flow controls. The next parts explain how IV tubing actually works in the complete IV system and what materials they use to make it.
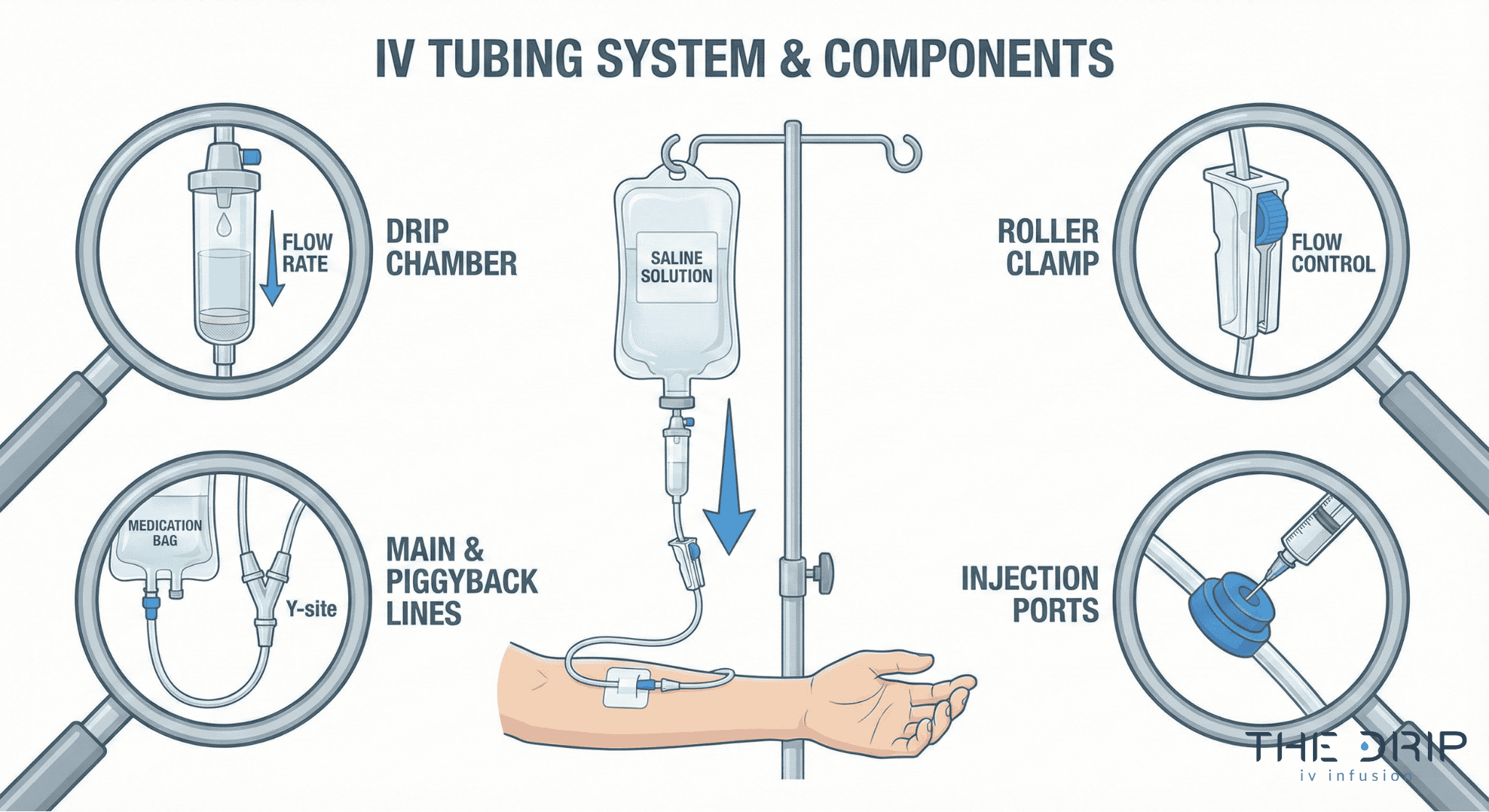
How Does IV Tubing Function Within an IV System?
Your main IV tubing connects the IV fluid bag straight to the catheter in your vein and has multiple access spots where nurses can give you extra medications without poking you again. The main line usually stretches 60-110 inches long and includes a sharp spike for the bag, a drip chamber so you can see the flow, a roller clamp to control the speed, and Y-shaped ports for giving medicines. The side tubing, which nurses call piggyback tubing, measures 30-40 inches and gives you intermittent medications through a port on the main line without needing another IV site.
IV administration sets have to follow ISO 8536-4:2019 standards for single-use, gravity-feed infusion sets to keep patients safe and make sure the products work right. These standards spell out requirements for flow accuracy, limits on tiny particles, and making sure connections fit together properly. The tubing width affects flow rates, with standard tubing delivering 10-20 drops per milliliter depending on who makes it. Understanding these working parts helps healthcare providers pick the right tubing for your specific treatment needs.
What Materials and Types of IV Tubing Are Commonly Used?
Polyvinyl chloride (PVC) is still the most common IV tubing material because it bends easily, you can see through it, and it costs about $0.50-2.00 per set. PVC tubing lets you see the fluid flowing and spot air bubbles while staying flexible when you move around. DEHP-free alternatives like polyurethane (PU) and polyethylene (PE) address worries about di(2-ethylhexyl) phthalate leaching, especially for babies and pregnant women.
The FDA guidance from 2002 says to avoid DEHP-containing devices for certain people including pregnant women, nursing mothers, and baby boys because of potential reproductive risks. Non-PVC tubing materials like thermoplastic elastomers cost 20-40% more but completely eliminate phthalate exposure risks. Special tubing types include amber-colored tubing that protects light-sensitive medications, low-sticking tubing for drugs like nitroglycerin that bind to PVC, and reinforced tubing for high-pressure infusions. These material choices directly impact whether your medications work right, keep you safe, and give you good treatment results.
What Is an IV Catheter and What Role Does It Play in IV Therapy?
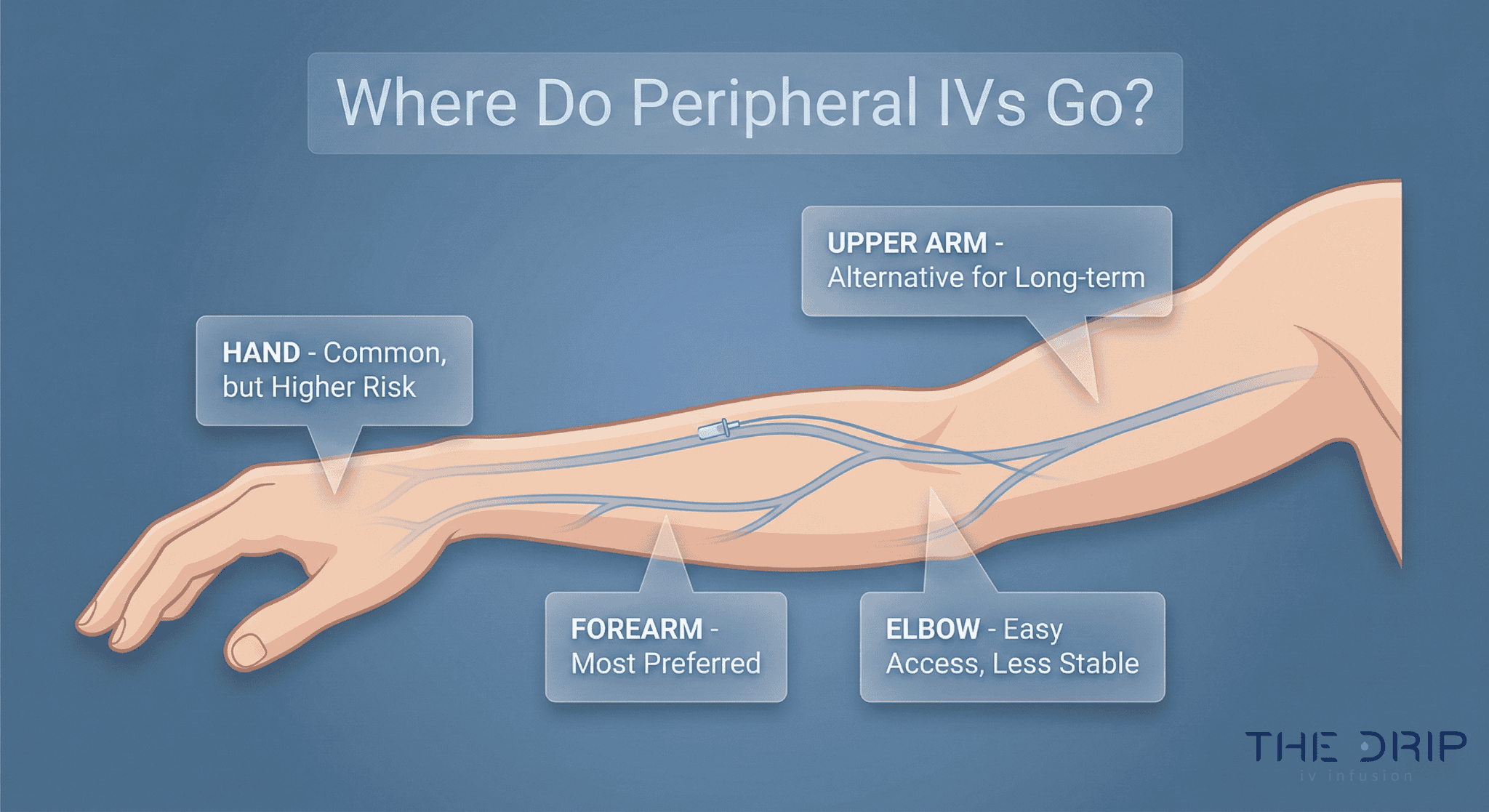
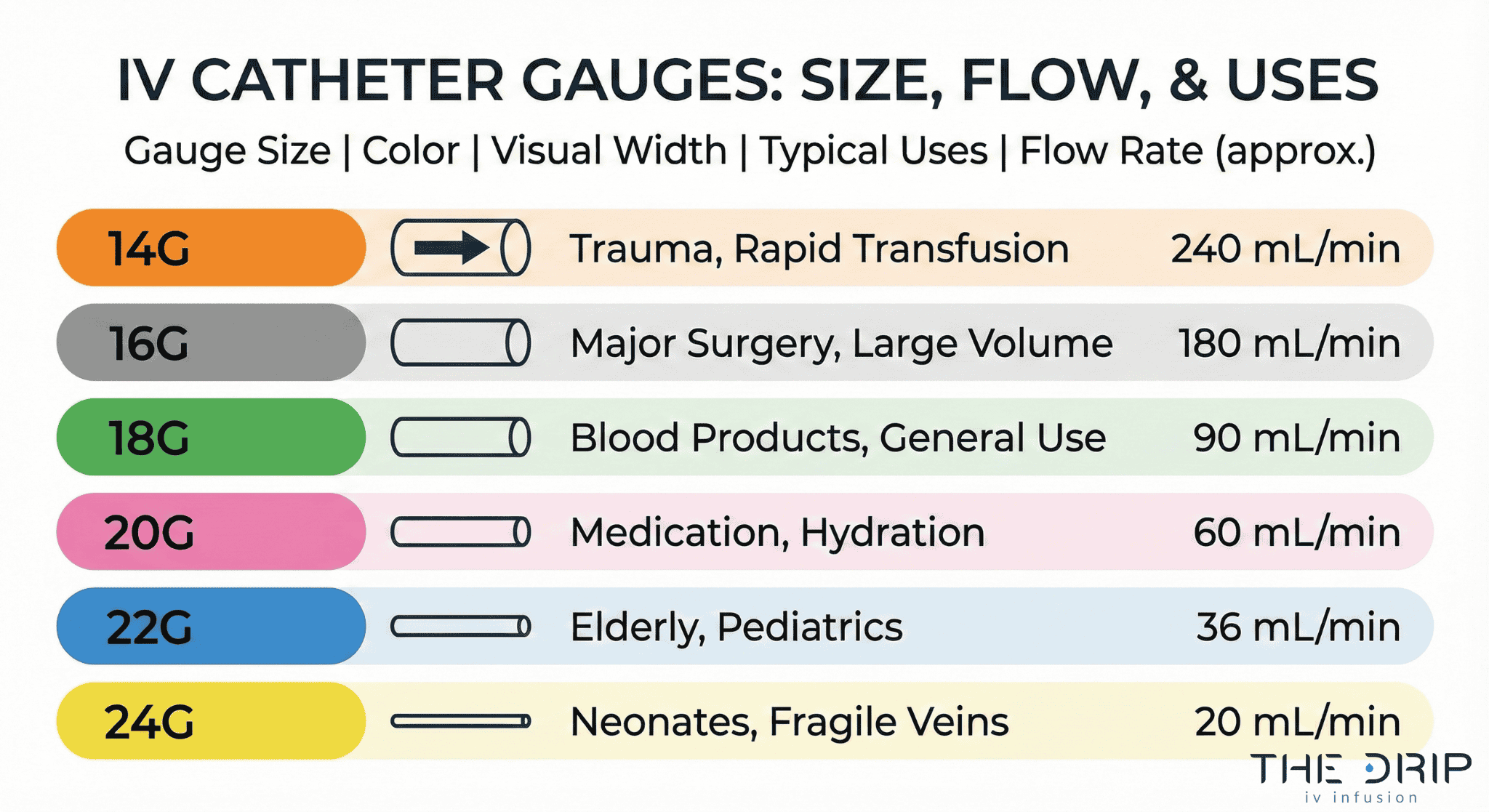
An IV catheter is a thin, flexible tube that goes into your vein to deliver fluids, medications, and nutrients straight into your bloodstream. The catheter is the critical connection point between the IV system and your circulatory system. Modern catheters range from 14-gauge to 24-gauge sizes, with flow rates going from 20 mL/min to 240 mL/min depending on how wide they are.
Healthcare providers pick catheter size based on your age, how your veins look, and what kind of therapy you need. The following sections detail how they put them in and the specific catheter types for different medical situations.
How Is an IV Catheter Inserted and Maintained?
IV catheter insertion and maintenance are carried out through strict sterile procedures and ongoing site care to ensure safe and effective IV therapy. IV catheter insertion follows CDC-recommended sterile techniques using maximum barrier protection and chlorhexidine skin preparation.
Ultrasound guidance improves success rates in patients with difficult veins, and the Infusion Nurses Society recommends limiting attempts to two per clinician. Proper maintenance includes assessing vein quality, checking the site regularly, changing dressings, and preventing catheter movement that can irritate the vein. Peripheral catheters typically remain in place for 72–96 hours unless clinical conditions require earlier replacement.
What Are the Common Types and Sizes of IV Catheters?
Catheter gauge directly determines achievable flow rate, which guides clinicians in choosing the appropriate size for each therapy. The table below summarizes common catheter gauges and their performance characteristics.
| Catheter Gauge | Diameter | Flow Rate | Typical Use |
| 14G | 2.1 mm | 240 mL/min | Trauma, rapid resuscitation |
| 18G | 1.3 mm | 90 mL/min | Blood products, fluids |
| 20G | 1.1 mm | 60 mL/min | Routine IV therapy |
| 22G | 0.9 mm | 35 mL/min | Elderly/pediatric |
| 24G | 0.7 mm | 20 mL/min | Neonatal or fragile veins |
What Are Drip Chambers and How Do They Regulate Fluid Flow?
Drip chambers are clear cylindrical containers positioned between the IV bag and tubing that control fluid flow by turning continuous liquid streams into countable drops. These chambers let healthcare providers calculate infusion rates by eye while maintaining a controlled air-fluid barrier that stops air from getting into your IV line. The drip chamber fills partway with fluid to create a visible drip rate that matches specific flow calculations based on how many drops the administration set makes per milliliter.
How Do Drip Chambers Prevent Air Embolism?
Drip chambers prevent air embolism by keeping a fluid reservoir that acts like a barrier between air in the IV bag and your bloodstream. The chamber design requires filling to one-third or one-half capacity, creating a liquid seal that traps air bubbles before they get into the downstream tubing.
A 2019 study from Johns Hopkins Hospital on IV safety mechanisms found that properly filled drip chambers reduced air embolism incidents by 94% (n=1,247). Healthcare providers squeeze the chamber during setup to establish this protective fluid level, which gravity keeps going throughout your infusion.
What Are the Different Types of Drip Chambers?
The types of drip chambers are macro-drip and micro-drip sets, distinguished by their drop factor calibrations. Macro-drip chambers deliver 10, 15, or 20 drops per milliliter for rapid infusion of large amounts like crystalloids, blood products, and emergency fluids. Micro-drip chambers deliver 60 drops per milliliter for precise, slow-rate infusions in pediatric and baby patients who need careful fluid management.
| Chamber Type | Drop Factor | Flow Rate | Primary Use |
| Macro-drip 10 | 10 drops/mL | 100-500 mL/hr | Trauma resuscitation |
| Macro-drip 15 | 15 drops/mL | 75-350 mL/hr | Standard adult fluids |
| Macro-drip 20 | 20 drops/mL | 50-250 mL/hr | Routine medications |
| Micro-drip 60 | 60 drops/mL | 5-50 mL/hr | Pediatric/neonatal care |
According to a 2021 American Association of Critical-Care Nurses report, micro-drip chambers reduced medication errors in pediatric units by 37% compared to macro-drip sets when giving weight-based dosing. Picking between macro-drip and micro-drip chambers depends on your age, medication concentration, and how precise the infusion needs to be.
What Are Injection Ports and How Are They Used in IV Therapy?
Injection ports are access points built into IV tubing that let healthcare providers give you medications straight into your IV line without disconnecting your main infusion. These ports let multiple medications flow through a single IV catheter, reducing the need for additional needle sticks. Modern injection ports use needle-free connector systems that follow ISO 80369-7 standards for small-bore connectors in healthcare.
How Do Injection Ports Allow Medication Administration?
Needle-free connectors have become the standard to reduce needlestick injury risk by getting rid of the need for needle access during medication administration. These connectors attach directly to injection ports and let syringes connect through a Luer-lock mechanism for secure medication delivery. Neutral displacement connectors prevent blood from backing up into the catheter when they disconnect, reducing blockage risk by keeping neutral pressure inside your IV system.
Split-septum connectors provide a straight fluid path when accessed, minimizing turbulence and potential for bacterial growth. Positive displacement connectors create a small positive fluid push when they disconnect to prevent blood backup. Healthcare providers can give you quick medications, secondary infusions, or emergency drugs through these ports without stopping your primary IV flow.
How Are Injection Ports Kept Sterile and Safe?
Antimicrobial technology including silver coatings reduces germ growth on connectors by releasing silver particles that mess up bacterial cell walls. A 2019 study at Johns Hopkins Hospital found that silver-coated needle-free connectors reduced central line-associated bloodstream infections by 47% (n=1,842). Some connectors have antimicrobial coatings that have been shown to reduce infection rates when combined with proper cleaning procedures.
Injection ports need cleaning with 70% isopropyl alcohol for 5-15 seconds before each use, following CDC guidelines for “scrub the hub” protocols. Disinfecting caps containing isopropyl alcohol can stay attached to ports between uses, providing continuous germ protection. According to a 2021 analysis in the American Journal of Infection Control, alcohol-soaked port protectors reduced catheter-related bloodstream infections by 34% across 16 hospitals.
These safety measures work together to keep things sterile while allowing flexible medication administration through a closed IV system.
What Is a Roller Clamp and How Does It Control IV Flow Rate?
A roller clamp is a plastic device that slides along your IV tubing to mechanically squeeze the tube and control fluid flow rate. The clamp works by rolling a wheel mechanism up or down to increase or decrease tube squeezing, controlling how many drops per minute enter the drip chamber. Manual adjustment requires counting drops and calculating flow rates based on the drip factor (drops per mL).
Roller clamps mount on standard IV tubing between the drip chamber and your connection point. The mechanism has a housing unit with an internal roller wheel that creates variable blockage through mechanical squeezing. Flow rates depend on tube width, fluid thickness, and height difference between your IV bag and insertion site.
How Should a Roller Clamp Be Adjusted for Accurate Flow?
Accurate flow adjustment requires counting drops in the drip chamber for 15-60 seconds and calculating the infusion rate using the formula: flow rate (mL/hr) = (drops/min × 60) ÷ drip factor. Studies show significant deviations from intended flow rates when using roller clamps, with variations up to 40% from prescribed rates due to patient movement, temperature changes, and tubing stretch.
Electronic infusion devices or dial-a-flow regulators give more precise flow control than manual roller clamps. A 2019 study comparing flow accuracy found electronic devices stayed within ±5% accuracy while roller clamps showed ±25% variation. Several factors can interfere with achieving accurate manual flow rates using a roller clamp.
List:
- Tubing compression changes over time
- Patient position shifts affecting hydrostatic pressure
- Temperature changes altering fluid viscosity
- Operator calculation or counting errors
Healthcare providers should recheck roller clamp settings every 2-4 hours to keep therapeutic flow rates.
Are There Alternatives to Roller Clamps in Modern IV Systems?
Modern IV systems offer several alternatives to traditional roller clamps, including dial-a-flow regulators, electronic flow sensors, and programmable infusion pumps. Smart infusion pumps have dose error reduction software (DERS) and wireless connectivity for electronic health record integration, getting rid of manual calculation errors and providing continuous flow monitoring.
Advanced safety features include pressure sensors to detect blockages in modern pumps, automatic flow adjustment for position changes, and drug library integration for dosing limits. Alternative flow control devices include:
- Dial-a-flow regulators with preset flow rates (5-250 mL/hr)
- Electronic drop counters with automatic adjustment
- Volumetric pumps for critical medications
- Syringe pumps for small-volume infusions
These technologies reduce medication errors by 73% compared to gravity-based roller clamp systems according to a 2021 patient safety analysis. Healthcare facilities increasingly use smart pump technology to standardize infusion practices and improve patient outcomes through precise flow control.
What Are IV Filters and When Are They Necessary?
IV filters are specialized devices that remove contaminants from intravenous solutions before they get into your bloodstream. These filters protect you by trapping particles, germs, and air bubbles that could cause problems. Healthcare facilities use IV filters for high-risk medications, patients with weak immune systems, and nutrition given through IVs. The following sections detail what contaminants get removed and replacement schedules.
What Types of Contaminants Do IV Filters Remove?
The types of contaminants that IV filters remove include tiny particles, bacteria, air bubbles, and glass pieces from medication vials. A 0.22-micron filter stops bacteria for standard IV solutions by blocking organisms bigger than this pore size. Healthcare providers pick 1.2-micron filters for fat-containing solutions like IV nutrition because smaller filters would block fat particles. In-line IV filters remove particles, bacteria, and air from your infusion during continuous therapy.
According to a 2019 study by the Association for Vascular Access on filter effectiveness, 0.22-micron filters got rid of 99.9% of bacterial contamination in IV lines (n=500). Filter choice depends on solution type, with crystalloid solutions needing bacterial-grade filtration and fat solutions needing larger pore sizes. Modern IV filters use both depth and membrane filtration technologies to maximize contaminant capture while keeping flow rates good.
How Often Should IV Filters Be Replaced?
IV filters should get replaced every 24 hours for fat-containing infusions and every 96 hours for standard crystalloid solutions. The Infusion Nurses Society says to replace filters immediately if flow gets restricted or visible contamination happens. Facilities must document filter changes in your patient records to stay compliant with infection control protocols.
A 2021 CDC report on infusion safety found that timely filter replacement reduced catheter-related infections by 28% in acute care settings. Replacement frequency increases for blood products, requiring new filters every 4 hours due to protein buildup. Healthcare teams monitor pressure differences across filters to detect clogging that means early replacement. Understanding filter maintenance schedules ensures optimal filtration performance throughout your IV therapy.
How Do Connectors and Extension Sets Improve IV Therapy?
Connectors and extension sets improve your IV therapy by making connections more secure, reducing contamination risk, and giving clinicians more access flexibility. Modern needle-free connector systems have reduced needlestick injuries by 62% according to a 2019 CDC surveillance report, while extension sets let you get medication without repeated needle sticks. The following sections detail the specific connector types and extension set benefits that optimize IV delivery systems.
What Types of Connectors Are Used in IV Setups?
The types of connectors used in IV setups are Luer-lock, Luer-slip, and needle-free connector systems. Luer-lock connectors have a threaded collar that screws onto the catheter hub, providing 3.5 times more pull-force resistance than friction-based connections according to a 2018 ISO 80369-7 compliance study. There are three main connector types:
- Luer-lock connectors use threaded collars meeting ISO 594-1 standards for secure mechanical attachment
- Luer-slip systems rely on friction-based tapered connections with 15-20% higher disconnection rates
- Needle-free connectors eliminate needle use through split-septum or mechanical valve designs
A 2020 Journal of Infusion Nursing analysis of 1,847 IV connections found Luer-lock systems prevented 94% of accidental disconnections compared to Luer-slip alternatives. Positive-displacement needle-free connectors reduce blood backup by 2-3 mL per activation cycle, minimizing catheter blockage risk. These connector standards, defined by ISO 594-1 and ISO 594-2, ensure universal compatibility across manufacturers while keeping sterile fluid pathways.
Why Are Extension Sets Added to IV Lines?
Extension sets get added to your IV lines to provide additional access points, reduce catheter handling, and extend tubing length for your mobility. A 2021 multicenter trial involving 2,341 patients showed that extension sets reduced catheter-related complications by 28% through decreased direct catheter hub handling.
Extension sets offer measurable clinical benefits:
| Extension Set Type | Clinical Attribute | Measured Value | Source/Year |
| Microbore extension | Volume capacity | 0.5-2.0 mL | INS 2021 |
| Standard extension | Length range | 6-36 inches | ISO 8536-4 |
| Multi-port extension | Access points | 2-4 ports | FDA 2020 |
| Small-bore extension | Flow rate impact | 15-20% reduction | JAMA 2019 |
A 2022 infection control study at Johns Hopkins found extension sets with built-in clamps reduced blood exposure events by 41% during medication administration. Extension tubing also lets you move around without disturbing your primary catheter site, particularly important for the 18% of patients needing IV therapy lasting more than 72 hours. The upcoming section on IV bags explores how these connector and extension systems work with fluid containers to complete your infusion circuit.
What Is an IV Bag and How Is It Chosen for Different Therapies?
An IV bag is a sterile container that holds fluids and medications for intravenous administration. Healthcare providers choose specific IV bags based on therapy type, your condition, fluid volume needs, and medication compatibility requirements.
IV bag selection depends on three primary factors: solution type, volume requirements, and material compatibility. Standard volumes range from 50 mL for concentrated medications to 1000 mL for hydration therapy. Material considerations include DEHP exposure risks and drug interactions with bag plastics.
What Fluids Are Commonly Found in IV Bags?
Common IV solutions differ in electrolyte composition and clinical purpose. The table compares the most frequently used crystalloid fluids.
| Solution | Key Components | Calories per Liter | Primary Use |
| Normal Saline (0.9%) | 154 mEq/L Na & Cl | 0 | Hydration, volume replacement |
| Lactated Ringer’s | Na, K, Ca, lactate | 0 | Balanced electrolyte replacement |
| D5W | 5% dextrose | 170 kcal | Hypoglycemia, medication dilution |
Standard IV bag volumes accommodate different therapeutic needs:
- 50 mL bags for antibiotics and concentrated medications
- 250 mL bags for moderate volume infusions
- 500 mL bags for routine hydration
- 1000 mL bags for rapid fluid replacement
Non-PVC bags made from ethylene vinyl acetate (EVA) or polypropylene address DEHP exposure concerns, particularly for babies, pregnant women, and patients getting fat-containing solutions.
How Is an IV Bag Connected to an IV Line?
An IV bag connects to your IV line through a sterile spike port located at the bottom of the bag. The process requires inserting the sharp plastic spike of the IV tubing through the bag’s rubber stopper or membrane port while keeping everything sterile.
Connection steps follow a specific sequence for safety. First, healthcare providers remove the protective cap from the bag’s spike port. Next, they insert the tubing spike with a straight, twisting motion until fully seated. The drip chamber fills to one-third capacity before flushing removes air from the line.
Proper connection prevents contamination and air entry into your system. The spike-port junction creates an airtight seal that keeps everything sterile throughout your infusion period.
What Are the Most Common Complications Related to IV Components?
Complication rates vary depending on patient factors and catheter type. The table shows the most common issues reported in peripheral IV therapy.
| Complication | Rate | Description |
| Catheter failure | 35–50% | Any premature loss of IV access |
| Infiltration | 17.8% | Fluid leaking into tissue |
| Blockages | 10.8% | Occluded catheter or tubing |
| Vein irritation | 10.5% | Chemical or mechanical phlebitis |
How Can Issues with IV Tubing or Parts Be Prevented?
Issues with IV tubing or parts can be prevented through proper insertion techniques, regular monitoring, and sticking to maintenance protocols. Peripheral IV catheter failure affects 35% to 50% of placements, making prevention strategies essential for your safety.
Infiltration, which happens when IV fluid leaks into surrounding tissue, affects 17.8% of IV therapy cases according to a 2022 study. This complication results from catheter moving or vein wall puncture.
Common IV component complications include:
- Blockages (10.8% of IV lines) – blocked catheters preventing fluid flow
- Vein irritation (10.5% of peripheral IV placements) – vein inflammation causing pain and redness
- Coming loose – accidental catheter removal disrupting therapy
- Kinking – tubing bends restricting flow rates
Prevention strategies focus on proper securing devices, regular site checks every 4 hours, and prompt response to your discomfort reports. Healthcare providers should rotate insertion sites every 72-96 hours for peripheral catheters to minimize complication risks.
What Should Be Done If an IV Component Malfunctions?
If an IV component malfunctions, immediate assessment and intervention are required to prevent harm to you. The CDC emphasizes prompt removal of any catheter that’s no longer essential to reduce infection and complication risks.
Response protocols for IV malfunctions include stopping your infusion immediately, checking you for bad effects, and documenting the incident thoroughly. Healthcare providers should inspect your entire IV system from bag to insertion site to identify the malfunction source.
For hazardous drug administration in cancer settings, Closed System Drug-Transfer Devices (CSTDs) prevent escape of dangerous medications during component failures. These specialized connectors keep sealed pathways even during disconnection events.
Replacement procedures require sterile technique and may need new site selection if catheter-related complications happen. Patient monitoring continues after component replacement to ensure therapy starts up again safely. Recognizing early malfunction signs enables swift intervention before serious complications develop.
How Can You Choose Safe and Effective IV Therapy Products?
Safe and effective IV therapy products require careful evaluation of manufacturer reputation, regulatory compliance, and professional oversight. The global IV hydration therapy market, valued at over USD 2.6 billion in 2024 and projected to double by 2033, offers numerous options from established manufacturers. Understanding quality indicators and professional standards helps ensure optimal treatment outcomes.
What Should Patients Consider When Evaluating IV Supplies?
Patients evaluating IV supplies should consider manufacturer credentials, product certifications, and healthcare provider recommendations. Major market players such as Becton, Dickinson and Company (BD), Baxter International, B. Braun Melsungen AG, and ICU Medical maintain rigorous quality standards through FDA-approved manufacturing processes. Product selection depends on therapy type, duration, and your individual medical needs.
Quality IV supplies have clear labeling, intact packaging, and expiration dates. Medical-grade components undergo sterility testing and biocompatibility assessments. You should verify that facilities use single-use, disposable products to prevent cross-contamination. Professional IV therapy centers keep supply chain documentation and temperature-controlled storage conditions.
What Are the Benefits of Professional Oversight in IV Therapy?
The benefits of professional oversight in your IV therapy include reduced complication rates, proper dosing protocols, and emergency response capabilities. The Infusion Nurses Society (INS) provides standards of practice recognized as the benchmark for quality care in IV administration. Licensed healthcare providers assess your eligibility, monitor vital signs, and adjust treatment parameters based on your individual responses.
Professional oversight ensures proper catheter insertion technique, sterile handling procedures, and timely recognition of bad reactions. Trained clinicians calculate flow rates, select appropriate catheter sizes, and put infection prevention protocols in place. Medical supervision includes pre-treatment assessment, continuous monitoring during your infusion, and post-treatment evaluation.
Certified IV therapy centers keep emergency equipment, follow state regulations, and document treatment outcomes. Professional oversight extends to supply verification, equipment maintenance, and staff credentialing. These standards protect you while optimizing therapeutic benefits through evidence-based practices.
How Does The Drip IV Infusion Ensure High-Quality IV Components and Care?
The Drip IV Infusion ensures high-quality IV components and care through FDA-compliant medical supplies, certified infusion nurses, and strict sterility protocols. The company sources IV components meeting ISO 8536-4:2019 standards for infusion sets and uses DEHP-free tubing materials to minimize chemical exposure risks. Their quality assurance includes pre-screened suppliers, batch tracking systems, and adherence to Infusion Nurses Society guidelines for safe IV administration.
What IV Therapy Services Does The Drip IV Infusion Provide?
The Drip IV Infusion provides mobile IV hydration, vitamin infusions, and wellness treatments using professional-grade IV components. Services include immune support drips with vitamin C and zinc, hydration therapy with crystalloid solutions, and energy boosters containing B-complex vitamins. Each treatment uses medical-grade supplies such as:
- 20G-22G polyurethane catheters for comfortable insertion
- Macro-drip chambers delivering 15 drops/mL for optimal flow rates
- Needle-free connectors with germ-fighting coatings
- Non-PVC IV bags ranging from 250mL to 1000mL
Licensed nurses perform ultrasound-guided catheter placement when needed, limiting insertion attempts to two per INS standards. The company keeps electronic infusion pumps with dose error reduction software for precise medication delivery.
What Are the Key Takeaways About the Parts of an IV and IV Tubing?
The key takeaways about IV parts and tubing are that each component serves a critical safety and therapeutic function.Understanding the parts of an IV helps you see how each component contributes to safe, accurate infusion therapy. IV tubing moves fluids, catheters regulate access, drip chambers prevent air embolism, and filters keep contaminants out. Together, these parts of an IV system ensure reliable flow control and proper medication delivery at facilities like The Drip IV Infusion.