When we lose more fluids than we take in, our bodies enter a state of dehydration that can range from mild thirst to life-threatening complications. We understand the concern that brings you here—whether you’re experiencing symptoms yourself, caring for a loved one, or simply want to be prepared. This comprehensive guide addresses your questions about IV therapy for dehydration, providing evidence-based information to help you make informed decisions about this increasingly common treatment option.
IV therapy for dehydration is a medical treatment that delivers fluids directly into the bloodstream through an intravenous line, bypassing the digestive system to achieve 100% absorption within 15 minutes compared to the 45-60 minutes required for oral fluid processing.
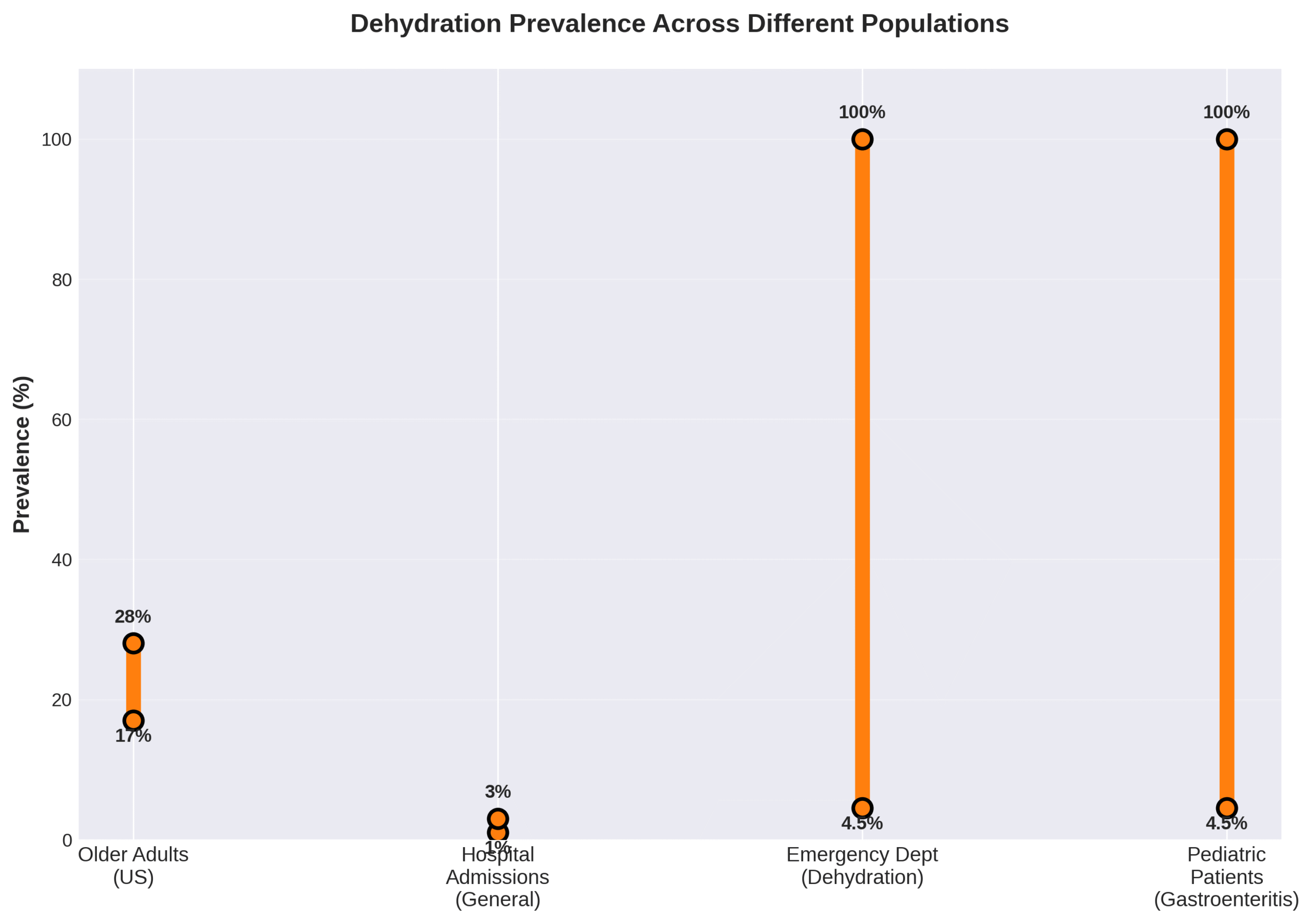
According to the Centers for Disease Control and Prevention (2016), dehydration affects 17% to 28% of older adults in the United States, with annual healthcare costs exceeding $1.14 billion for dehydration-related hospital admissions.
As Dr. Joshua Septimus from Houston Methodist explains, “IV therapy is a routine procedure that’s incredibly standardized and safe in the clinical setting when administered by professionals in a medical-grade facility.”
Key Takeaways:
• Dehydration occurs when fluid loss exceeds intake, with prevalence ranging from 17-28% in older adults
• IV therapy provides immediate relief through 100% bioavailability versus 55% absorption with oral hydration
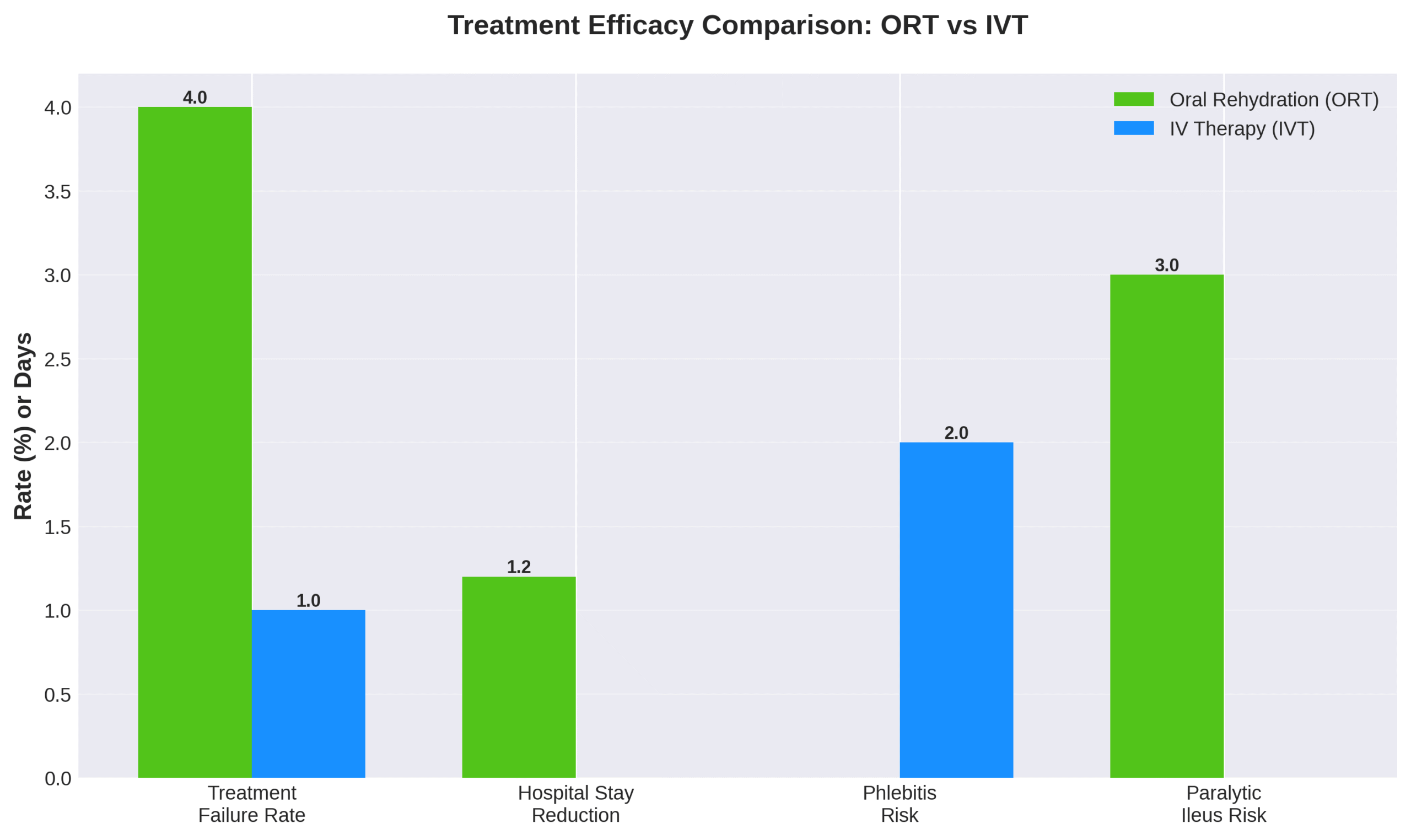
• Treatment efficacy shows IV therapy with 1.3% failure rate compared to 4.9% for oral rehydration
• Common IV fluids include 0.9% normal saline and balanced crystalloid solutions like Lactated Ringer’s
• Medical necessity determines appropriateness, with costs ranging from $100-500 per session
• Safety requires administration by trained professionals following established clinical standards
• Both benefits and risks exist, making professional evaluation essential for treatment decisions
This article synthesizes the latest clinical research and expert insights to explore how IV therapy works differently from oral hydration, who benefits most from this treatment, what to expect during a session, and how to evaluate whether it’s right for your specific situation. We’ll examine the science behind rapid rehydration while addressing common misconceptions about wellness IV therapy versus medically necessary treatment.
Practical Tip: Before considering IV therapy, assess your hydration status by monitoring urine color (pale yellow indicates adequate hydration), checking for symptoms like dizziness or dry mouth, and attempting oral rehydration first unless you have persistent vomiting or severe symptoms requiring immediate medical attention.
As we explore the mechanisms, applications, and considerations surrounding IV therapy for dehydration, you’ll gain the knowledge needed to recognize when this treatment is truly beneficial versus when simpler hydration methods suffice. Let’s begin by understanding the fundamental causes and progression of dehydration itself.
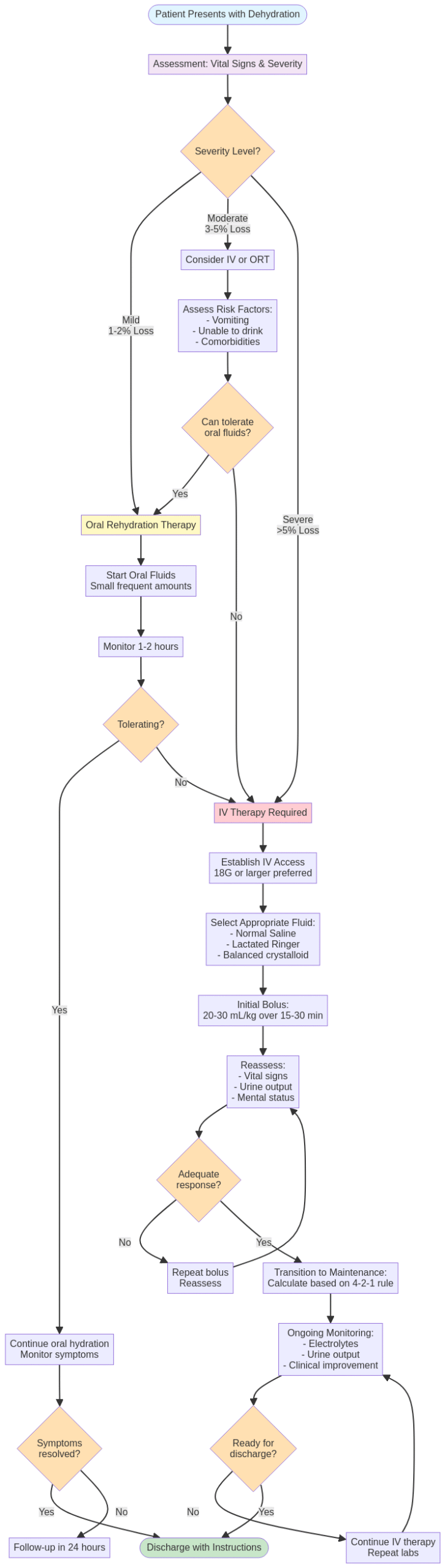
Why Does Dehydration Occur and What Are Its Common Causes?
Dehydration occurs when the body loses more fluids than it takes in. Low fluid intake and increased fluid loss are the primary causes. Among older adults in the United States, dehydration prevalence ranges from 17% to 28%. This condition accounts for 1% to 3% of all hospital admissions nationally, with rates climbing during heat waves. The annual healthcare cost for primary dehydration diagnoses exceeded $1.14 billion in 1999. Older individuals are 20% to 30% more prone to developing dehydration compared to younger adults.
Common causes include gastrointestinal fluid loss through diarrhea and vomiting, inadequate fluid intake, excessive sweating, and fever. Medications such as diuretics and laxatives significantly increase risk. Chronic conditions including diabetes mellitus, renal disease, and gastrointestinal disorders compound dehydration vulnerability. Understanding these causes helps identify when IV therapy for dehydration becomes necessary, especially for those unable to maintain adequate oral hydration.
What Are the Signs and Symptoms of Mild, Moderate, and Severe Dehydration?
The signs and symptoms of mild, moderate, and severe dehydration progress from simple thirst to life-threatening complications. Mild dehydration at 1-2% body weight loss causes thirst, fatigue, and weakness. Athletes generally tolerate this level well. Moderate dehydration at 3-5% body weight loss leads to decreased urine output, dry mouth, dizziness, and impaired cognitive performance affecting psychomotor and memory skills.
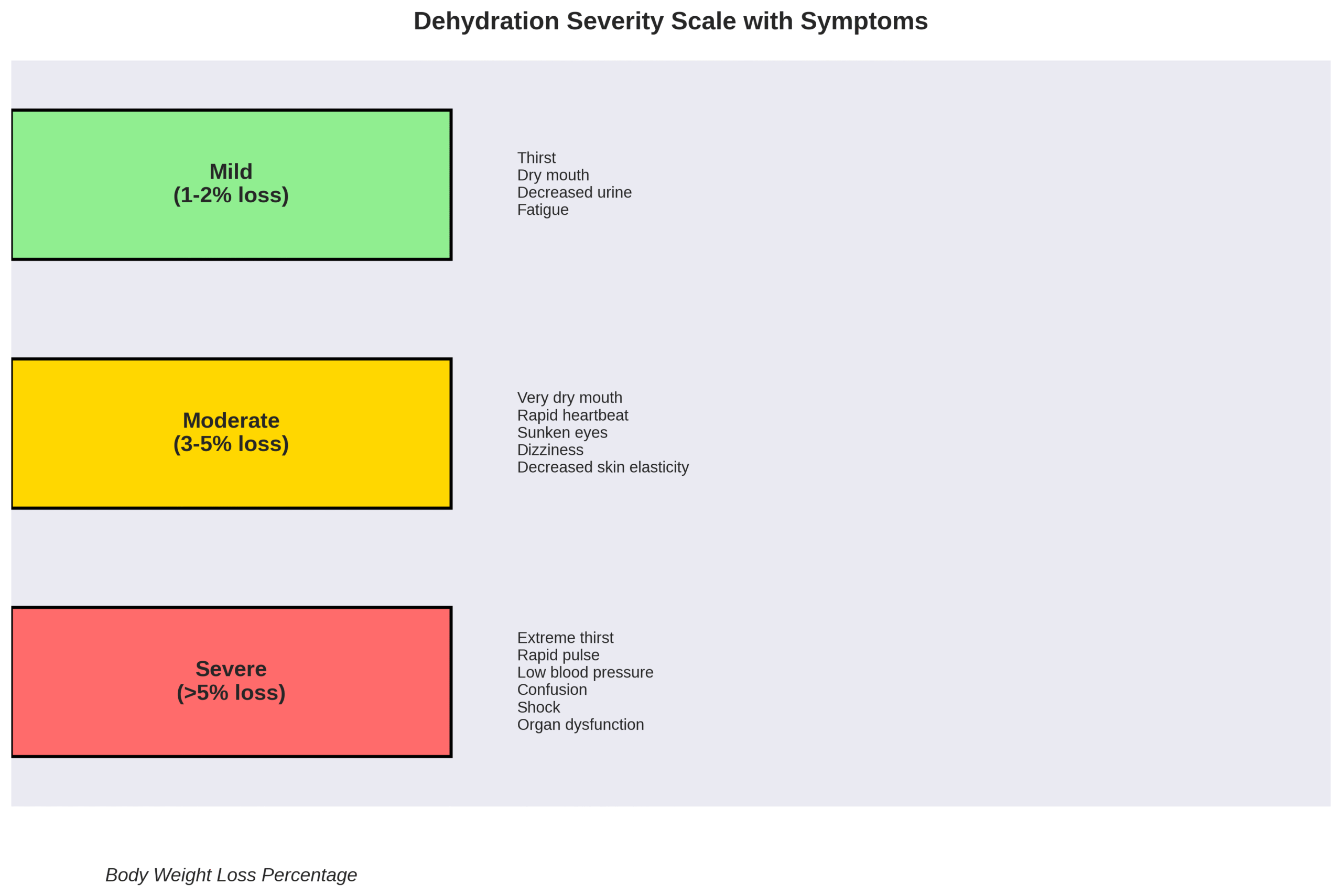
Severe dehydration exceeding 5% body weight loss results in confusion, hypotension, hypovolemic shock, neurological impairment, and multiple organ dysfunction. A fluid deficit of 4% creates more severe impacts on physical and cognitive performance than lower levels. In athletes, dehydration greater than 2% body weight loss negatively affects performance. These symptoms require immediate medical intervention as severity increases.
How Can Dehydration Affect Overall Health and Wellbeing?
Dehydration by 1-2% impairs cognitive performance and impacts psychomotor and memory skills. In older adults, dehydration leads to acute confusion, constipation, urinary tract infections, fatigue, falls, and delayed wound healing. Hospital stays lengthen, healthcare costs increase, and morbidity and mortality rates rise with dehydration.
Severe dehydration causes acute kidney injury, electrolyte imbalances, and multiple organ dysfunction. During exercise, metabolic demand produces heat with 80% of heat loss occurring through sweat vaporization in hot, dry conditions. Complications include hyperchloremia, metabolic acidosis, and decreased glomerular filtration rate. Among elite triathletes, muscle cramping due to dehydration represents one of the most common reasons cited for not finishing races.
What Factors Increase the Risk of Dehydration?
The factors that increase dehydration risk span age, medications, medical conditions, and environmental factors. According to CDC data, men aged 60+ consume 2.92 L daily, roughly 0.8 L less than adequate intake. Medications including diuretics, laxatives, and certain antihypertensive drugs significantly elevate risk. Immobility, impaired thirst mechanism, diminished cognition, and dependence on caregivers for fluid intake create major vulnerabilities in elderly populations.
Diabetes mellitus, renal disease, and polypharmacy compound dehydration risks. Institutionalized settings show higher dehydration rates compared to community-dwelling individuals.
Environmental factors such as heat waves and extreme weather dramatically increase risk. Athletes face elevated risk due to sweat loss influenced by body weight, genetics, heat acclimatization, and metabolic efficiency. These overlapping factors often necessitate IV therapy intervention when oral rehydration proves insufficient.
How Does IV Therapy Rehydrate the Body Differently Than Oral Hydration?
IV therapy rehydrates the body differently than oral hydration through direct bloodstream delivery that bypasses the digestive system entirely. IV fluids achieve 100% absorption compared to approximately 55% absorption with oral hydration. The direct intravascular delivery allows fluids to take effect within 15 minutes versus 45-60 minutes for oral fluids to process through the digestive system. IV rehydration bypasses the oropharyngeal reflex and associated digestive enzymes and hormones.
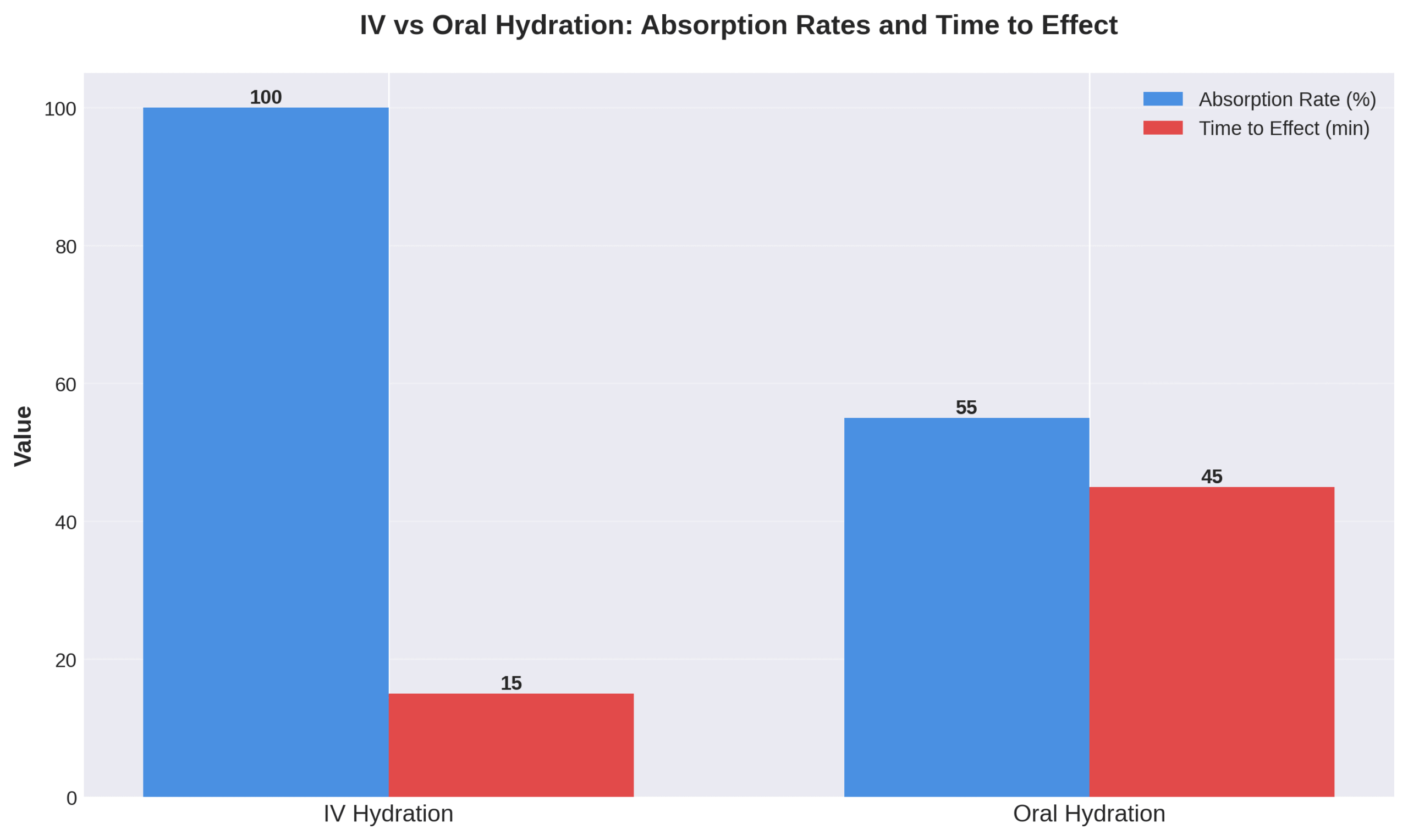
For severe dehydration or shock, IV therapy demonstrates lower failure rates of 1.3% compared to 4.9% for oral rehydration therapy. IV therapy enables precise control of fluid and electrolyte delivery, especially when oral administration is impossible or impaired. The following sections detail the key components, timing, and types of IV fluids used for optimal rehydration.
What Are the Key Components of IV Therapy for Dehydration?
The key components of IV therapy for dehydration are crystalloid and colloid fluids, with crystalloids being first choice for most indications. Crystalloid fluids contain aqueous solutions of mineral salts and small water-soluble molecules that approximate plasma concentrations. Most commonly used IV fluids include 0.9% sodium chloride (normal saline) with or without potassium additions. IV solutions contain small amounts of salt or sugar (dextrose, glucose, levulose) dissolved in sterile water. Balanced crystalloid solutions contain buffered molecules such as lactate, acetate, and gluconate that metabolize to bicarbonate to maintain physiologic pH.
Standard maintenance fluid calculation follows the “4-2-1” rule:
- 4 mL/kg/h for first 10 kg body weight
- 2 mL/kg/h for next 10 kg
- 1 mL/kg/h for weight over 20 kg
Volume requirements vary based on body composition, dehydration level, cardiac output status, daily urine output, and blood pressure.
How Quickly Can IV Fluids Relieve Symptoms of Dehydration?
IV fluids relieve symptoms of dehydration within 15 minutes of administration by directly entering the bloodstream. Several studies demonstrate more rapid rehydration with IV fluid compared to oral methods, though benefits are generally transient and small. The 2018 Surviving Sepsis Campaign Guidelines recommend 30 mL/kg crystalloid within 1 hour for hypotension or lactate ≥4 mmol/L. Rapid infusion for severe dehydration requires pressure apparatus and large-bore IV cannulas (18 gauge or larger) or central access. Clinical improvement typically occurs within the first hour of IV therapy initiation for moderate to severe dehydration. Complete rehydration is achieved within 2-4 hours depending on severity and fluid deficit. IV prehydration and rehydration in athletes serves as an ergogenic aid to achieve euhydration more effectively than oral methods.
What Types of IV Fluids Are Used for Dehydration?
The types of IV fluids used for dehydration include crystalloid solutions, with 0.9% NaCl (Normal Saline) being most frequently used. Normal saline contains 154 mmol/L chloride, higher than human serum levels of 98-106 mmol/L. Lactated Ringer’s/Hartmann Solution provides a balanced approach with sodium (130-131 mEq), chloride (109-111 mEq), lactate (28-29 mEq), potassium (4-5 mEq), and calcium.
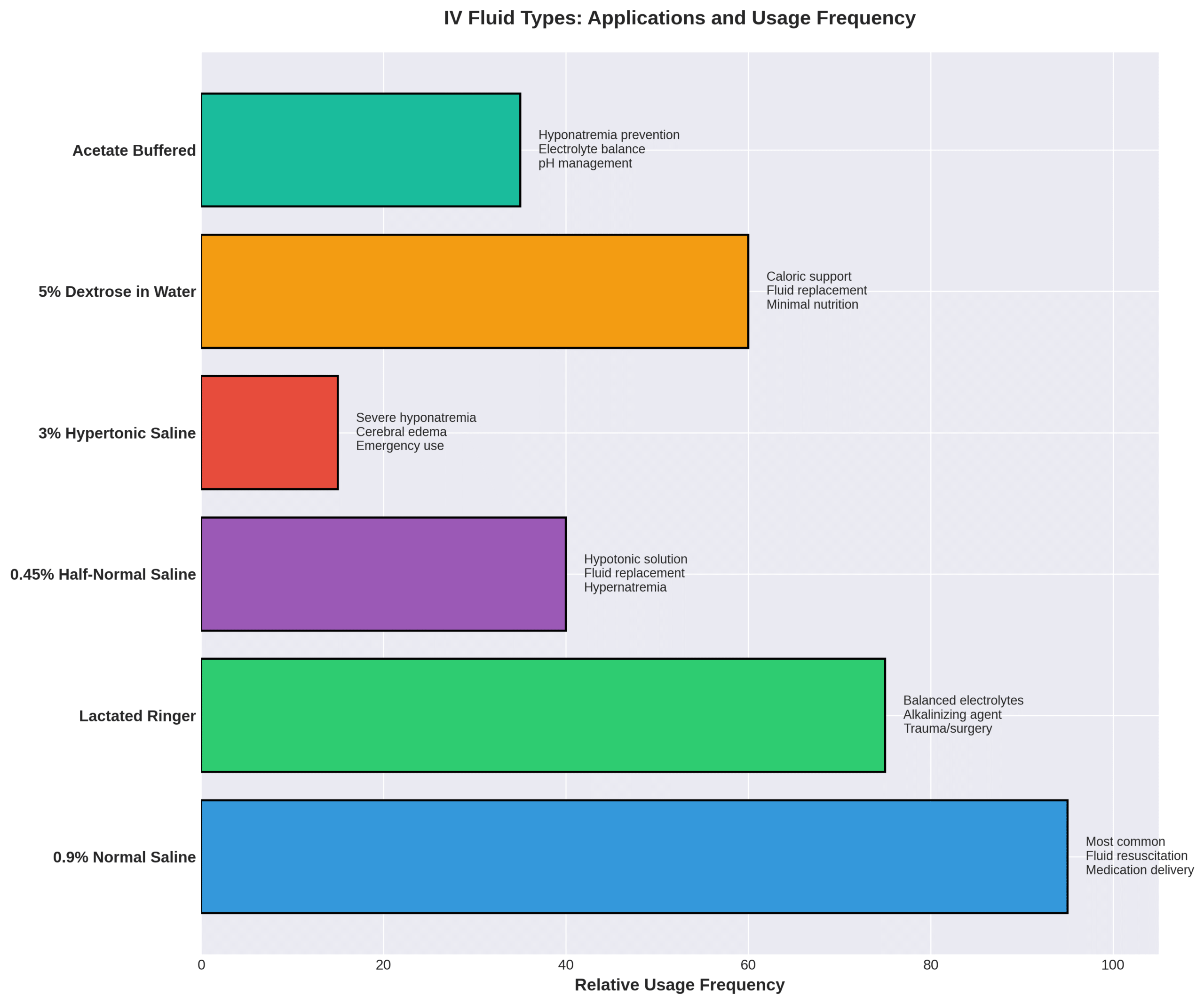
| Fluid Type | Composition | Primary Use |
| 0.9% NaCl | 154 mmol/L chloride | Most common crystalloid |
| 0.45% NaCl | Half-strength saline | Hypotonic replacement |
| Lactated Ringer’s | Balanced electrolytes | Physiologic replacement |
| 3-5% NaCl | Hypertonic solution | Emergent hyponatremia |
| 5-10% Dextrose | Sugar in water | Fluid and calories |
Acetate and gluconate buffered solutions serve as alkalinizing agents with metabolism to bicarbonate. The SMART Trial showed balanced crystalloid solutions resulted in lower death rates compared to normal saline in critically ill patients. Hypertonic solutions remain reserved for emergent replacement of serum solutes, particularly hyponatremia with neurologic symptoms.
Who Can Benefit Most from IV Therapy for Dehydration?
IV therapy for dehydration shows vastly different utilization rates across patient populations. Pediatric patients receive IV rehydration at rates from 4.5% to 100% depending on condition severity, with gastrointestinal fluid loss being the primary indication. Adult IV therapy prevalence ranges from 1.5% to 100%, encompassing broader conditions such as fever, diarrhea, drug intoxication, and hypercalcemia.
Patients with severe dehydration or shock derive the greatest benefit from IV therapy. A clinical comparison reveals IV therapy has lower failure rates (1.3%) compared to oral rehydration (4.9%). Primary candidates include individuals unable to tolerate oral fluids due to vomiting, altered mental status, or gastrointestinal disorders. Terminal care patients lacking adequate oral intake receive IV hydration for comfort and symptom management.
Specific medical conditions necessitate IV fluid therapy. These include acute renal failure, hyponatremia, hypercalcemia, acute pancreatitis, and sepsis. Emergency department data shows 100% IV therapy utilization for patients with moderate to severe dehydration from viral gastroenteritis. The following sections examine specific populations and their unique IV therapy considerations.
Is IV Therapy Recommended for Athletes, Travelers, or The Elderly?
IV therapy recommendations vary significantly across these populations. Athletes experiencing dehydration exceeding 2% body weight loss may benefit from IV therapy, though routine use cannot be recommended as best practice for most athletes. The World Anti-Doping Agency (WADA) prohibits IV infusions exceeding 50 mL per 6 hours in healthy athletes except during legitimate hospital admissions. The NCAA wrestling program specifically prohibits artificial rehydration including IV therapy as a weight-management violation.
Older adults represent a high-need population with 17-28% dehydration prevalence. Institutionalized seniors with limited fluid access particularly benefit from IV therapy. Mobile IV therapy provides rapid hydration that addresses age-related deficiencies more effectively than oral supplements.
Travelers experiencing jet lag or altitude sickness sometimes seek IV therapy, though clinical evidence supporting benefits in healthy individuals remains limited. IV therapy should be reserved for high-level athletes with documented dehydration symptoms in well-monitored settings. These targeted applications ensure appropriate use while avoiding unnecessary medical interventions.
Can IV Hydration Help With Illnesses or Hangovers?
IV hydration addresses the dehydration component of hangovers, though experts emphasize it’s “not a miracle cure” and the body’s detoxification system simply needs time. Dr. Joshua Septimus states clearly: “There’s no evidence that getting an IV bag full of vitamin C will help stave off illness.” Research shows mild to moderate hangover symptoms including fatigue, thirst, and headache following IV alcohol exposure in controlled studies.
Illness-related dehydration from fever, vomiting, or diarrhea responds effectively to IV therapy for fluid and electrolyte replacement. Recent COVID-19 studies treating patients with vitamin C IV therapy failed to demonstrate any benefit. Cancer patients benefit from IV hydration to maintain fluid status during treatment when oral intake becomes compromised.
Emergency department data reveals 100% IV therapy utilization for gastroenteritis patients admitted with moderate dehydration. This high utilization rate reflects IV therapy’s effectiveness for illness-induced fluid losses rather than preventive or wellness applications.
When Should You Seek Medical Attention for Dehydration?
Medical attention for dehydration becomes necessary under specific circumstances. Severe dehydration presenting with confusion, hypotension, or altered mental status requires immediate medical intervention. Persistent vomiting preventing fluid retention warrants medical evaluation for IV therapy. Hypovolemic shock signs including rapid heart rate, low blood pressure, and decreased urine output demand emergency treatment.
Neurological symptoms such as seizures or loss of consciousness related to dehydration require immediate IV intervention. Children experiencing treatment failure after oral rehydration therapy (4.9% failure rate) need medical evaluation for IV fluids. Elderly patients presenting with acute confusion, falls, or significant functional decline related to dehydration require medical assessment.
Dehydration persisting more than 3 days despite oral rehydration attempts should prompt medical consultation. These guidelines help identify when professional medical intervention supersedes home management strategies.
What Is the IV Therapy Session Like for Dehydration Treatment?
An IV therapy session for dehydration treatment is a clinical procedure involving direct fluid administration into the bloodstream through intravenous access. Healthcare professionals begin by assessing vital signs, reviewing medical history, and evaluating dehydration severity. The provider selects an appropriate IV access site, typically in the arm, and inserts a cannula using sterile technique.
Treatment parameters depend on clinical assessment. Fluid volumes range from 500-1000 mL, with administration rates varying from rapid bolus for severe dehydration to slower maintenance rates for mild cases. Patients remain seated or reclined while healthcare staff monitor vital signs and treatment response. Documentation includes fluid intake, adverse reactions, and clinical improvement throughout the session. The session concludes with reassessment of hydration status and determination of additional therapy needs.
What Should You Expect During a Typical IV Hydration Appointment?
A typical IV hydration appointment begins with comprehensive medical history review, including current medications, allergies, and dehydration symptoms. Healthcare providers monitor vital signs including blood pressure and heart rate. Laboratory tests for electrolyte levels may be performed based on clinical indication.
The IV insertion process uses an 18-20 gauge needle placed in an arm vein. Patients experience minimal discomfort during insertion. During infusion, patients can relax, read, or use electronic devices while fluid enters the bloodstream. Healthcare staff periodically check flow rates and monitor for complications.
Treatment facilities provide comfortable seating and temperature-controlled environments. Upon completion, staff remove the IV catheter, apply pressure to prevent bleeding, and place a bandage over the insertion site. The entire process prioritizes patient comfort while ensuring effective hydration delivery.
How Long Does an IV Therapy Session Take?
IV hydration sessions typically last 30-60 minutes for standard 500-1000 mL fluid administration. According to the 2018 Surviving Sepsis Campaign Guidelines, rapid rehydration protocols deliver 30 mL/kg within 1 hour for severe dehydration. Mobile IV therapy appointments require 45-90 minutes including travel, setup, and treatment.
Emergency department IV rehydration may extend 2-4 hours based on severity and initial treatment response. Maintenance IV fluids for a 100 kg patient calculate at 140 mL/h, requiring approximately 7 hours for 1000 mL administration. Add-on vitamins or medications extend sessions by 15-30 minutes.
Post-treatment observation periods of 15-30 minutes allow monitoring for delayed reactions. Total appointment duration depends on dehydration severity, fluid volume requirements, and individual response to treatment.
Are There Any Guidelines to Follow Before and After the Procedure?
Before IV therapy, patients must disclose all medications, allergies, and medical conditions, particularly kidney or heart disease. Hydration status assessment may require avoiding excessive fluids immediately before appointments. Patients should wear comfortable clothing with easy arm access.
After treatment, the insertion site requires clean and dry maintenance for 24 hours to prevent infection. Patients should monitor for infiltration signs including swelling, pain, or coolness at the insertion site. Maintaining adequate oral hydration following IV therapy sustains treatment benefits.
Emergency symptoms requiring immediate medical attention include shortness of breath, chest pain, or severe headache. These guidelines ensure safe IV therapy administration and optimal treatment outcomes while minimizing complication risks.
What Are the Benefits and Potential Risks of IV Therapy for Dehydration?
The benefits and potential risks of IV therapy for dehydration involve direct vascular delivery advantages balanced against medical complications. IV therapy achieves 100% bioavailability versus 55% absorption through oral hydration. Clinical studies demonstrate failure rates of 1.3% for IV therapy compared to 4.9% for oral rehydration therapy. Symptom relief occurs within 15 minutes rather than 45-60 minutes required for oral fluids.
A 2012 meta-analysis of 526 participants across 6 trials found hospital stays reduced by 1.20 days for IV therapy patients versus oral rehydration. IV therapy enables treatment when vomiting, altered consciousness, or gastrointestinal dysfunction prevents oral intake. Direct intravascular delivery provides precise fluid and electrolyte control in critically ill patients. The upcoming subsections examine specific advantages, risks, and safety considerations.
What Advantages Does IV Therapy Offer Over Other Hydration Methods?
The advantages IV therapy offers over other hydration methods are bypassing digestive barriers and enabling rapid, controlled fluid delivery. IV fluids enter tissues immediately without gastrointestinal processing. Higher fluid volumes deliver quickly without causing nausea or distress. Patients with impaired swallow reflexes or aspiration risks receive reliable hydration through IV access. Medications, vitamins, and electrolytes administered simultaneously with precise dosing control.
The 2018 SMART Trial demonstrated balanced crystalloid IV solutions reduced mortality compared to normal saline in critically ill patients. Severe dehydration responds to IV therapy when oral rehydration proves too slow. Surgical patients maintaining nil per os status continue hydration through IV access during procedures.
Are There Any Side Effects or Contraindications to Be Aware Of?
The side effects and contraindications to be aware of include metabolic disturbances and vascular complications. Hyperglycemia and hyponatremia cause osmotic diuresis, increasing cerebral edema risk. Phlebitis occurs with a number needed to treat of 50 (95% CI: 25 to 100) compared to oral rehydration. Volume overload threatens patients with congestive heart failure or kidney impairment. Normal saline containing 154 mmol/L chloride causes hyperchloremia and metabolic acidosis. Kidney disease, heart problems, or severe allergies contraindicate IV nutrient therapy without supervision. Minor complications include pain, swelling, bruising, and injection site scarring. Serious risks encompass air embolism, bloodstream infection, soft tissue infiltration, and arterial puncture.
How Safe Is IV Therapy When Administered by Trained Professionals?
IV therapy administered by trained professionals is a routine, standardized procedure following established safety protocols. The Infusion Nurses Society standards provide comprehensive guidelines supported by 1,184 citations. Many states adopted USP 797 as the minimum standard for IV hydration practices. Licensed professionals reduce infection, thrombophlebitis, and fluid selection errors through proper training.
California requires 51% physician ownership of IV therapy clinics for regulatory compliance. Qualified staff monitoring prevents electrolyte imbalances and fluid overload complications. Dr. Septimus emphasizes hospital IV therapy occurs “by professionals in a medical-grade facility” ensuring safety standards. Professional administration transforms IV therapy into a controlled medical procedure with minimal risks when protocols are followed.
How Can You Evaluate if IV Therapy for Dehydration Is Right for You?
IV therapy for dehydration is right for you when medical necessity exists, not wellness preference. Healthy individuals maintain hydration through oral intake without IV intervention. A 2021 clinical review by Dr. Joshua Septimus at Houston Methodist states definitively: “If you’re healthy, do you need to get your hydration from an IV? The answer is a resounding, ‘No.'” Cost ranges from $100-$500 per session in the United States.
Insurance rarely covers wellness IV therapy. Severe dehydration with confusion, hypotension, or persistent vomiting requires IV treatment. Mild dehydration resolves with oral rehydration. Medical conditions such as heart disease, kidney disease, or electrolyte imbalances may contraindicate IV therapy. Healthcare provider assessment determines whether inability to maintain oral hydration justifies IV therapy risks and costs. The following subsections explore evaluation factors and provider selection criteria.
What Factors Should You Consider Before Choosing IV Hydration?
The factors to consider before choosing IV hydration are insurance coverage, cost, medical history, and risk-benefit analysis. Insurance excludes IV therapy as optional/elective wellness treatment. Pricing varies by provider: Mobile IV Medics charges $199 minimum, Mobile IV Nurses ranges $115-$625, and NYC providers charge $150-$350. Medical contraindications include kidney disease, heart conditions, and certain medications. Payment alternatives include HSA/FSA accounts, membership programs offering 20-30% discounts, and package deals. Risk analysis weighs complications against expected benefits. Geographic location determines service availability and pricing. Treatment requires 30-90 minutes including setup, infusion, and monitoring. Alternative payment methods help offset out-of-pocket expenses when insurance denies coverage.
How Do You Find a Qualified IV Therapy Provider?
A qualified IV therapy provider meets state regulations, follows safety standards, and employs licensed medical professionals. California requires 51% physician ownership of IV clinics. USP 797 standards serve as minimum requirements in many states. INS (Infusion Nurses Society) standards guide best practices with 1,184 evidence-based citations. Staff must include licensed RNs, NPs, PAs, or MDs trained in IV insertion and monitoring. Medical-grade facilities maintain sterility protocols for fixed locations.
Mobile services require equivalent safety standards. Emergency protocols and physician oversight ensure proper adverse reaction management. Liability insurance and documentation practices protect both provider and patient. These verification steps ensure safe, professional IV therapy administration aligned with medical standards.
How Can The Drip IV Infusion Support Your Hydration and Wellness Goals?
The Drip IV Infusion supports hydration and wellness goals through direct intravenous fluid delivery that achieves 100% bioavailability compared to 55% oral absorption. This method bypasses the digestive system entirely, delivering fluids and nutrients directly into the bloodstream within 15 minutes.
A 2018 review of IV therapy protocols demonstrates that direct intravascular delivery enables precise control of fluid and electrolyte balance, particularly beneficial for individuals with impaired oral intake or absorption issues.
The following sections explore The Drip IV Infusion’s specific treatment options and essential considerations for IV hydration therapy.
What IV Therapy Options Does The Drip IV Infusion Offer for Dehydration?
The Drip IV Infusion offers customized IV therapy protocols using crystalloid solutions, primarily 0.9% normal saline and balanced solutions like Lactated Ringer’s. Treatment protocols follow the standard “4-2-1” maintenance fluid calculation: 4 mL/kg/h for the first 10 kg, 2 mL/kg/h for the next 10 kg, and 1 mL/kg/h for weight over 20 kg. Session durations range from 30-60 minutes for standard 500-1000 mL fluid administration.
The Drip IV Infusion provides mobile and clinic-based services with trained medical professionals monitoring vital signs throughout treatment. Protocols include initial assessment of dehydration severity, selection of appropriate IV fluids based on individual needs, and post-treatment evaluation. According to 2021 INS standards, proper administration requires sterile technique and continuous monitoring for adverse reactions.
What Are the Key Takeaways About IV Therapy for Dehydration?
The key takeaways about IV therapy for dehydration are:
- IV therapy delivers 100% bioavailability with effects within 15 minutes versus 45-60 minute oral absorption
- Dehydration affects 17-28% of older adults and accounts for 1-3% of US hospital admissions with costs exceeding $1.14 billion annually
- Treatment failure rates favor IV therapy (1.3%) over oral rehydration (4.9%) for moderate to severe dehydration
- Most commonly used fluids include 0.9% normal saline and balanced crystalloid solutions like Lactated Ringer’s
- Costs range from $100-$500 per session and are rarely covered by insurance for wellness purposes
- Medical professionals emphasize IV therapy unnecessary for healthy individuals who can maintain hydration orally
- Safety requires administration by trained professionals following established standards to minimize risks of complications
A 2018 SMART Trial involving critically ill patients found balanced crystalloid solutions resulted in lower mortality rates compared to normal saline. These evidence-based findings guide The Drip IV Infusion’s approach to safe, effective hydration therapy tailored to individual wellness needs.
