We understand you’re searching for safe and effective ways to support your health during pregnancy. If you’re experiencing persistent nausea, dehydration, or nutritional concerns that oral supplements haven’t resolved, you’ve come to the right place. Our comprehensive guide addresses the critical questions expectant mothers have about IV therapy, backed by the latest medical research and clinical guidelines.
IV therapy for pregnancy is a medical treatment that delivers fluids, vitamins, and minerals directly into the bloodstream through an intravenous line, bypassing the digestive system to provide immediate hydration and nutritional support for expecting mothers experiencing severe symptoms or deficiencies. According to the Royal College of Obstetricians and Gynaecologists (2024), normal saline (0.9% NaCl) with additional potassium chloride represents the most appropriate intravenous hydration protocol for pregnant women, with administration guided by daily monitoring of electrolytes. In 2024, researchers at Nature Scientific Reports found that pregnant women receiving IV iron were 39% less likely to experience adverse events compared to oral iron supplementation, based on analysis of 13,909 women across 34 studies.
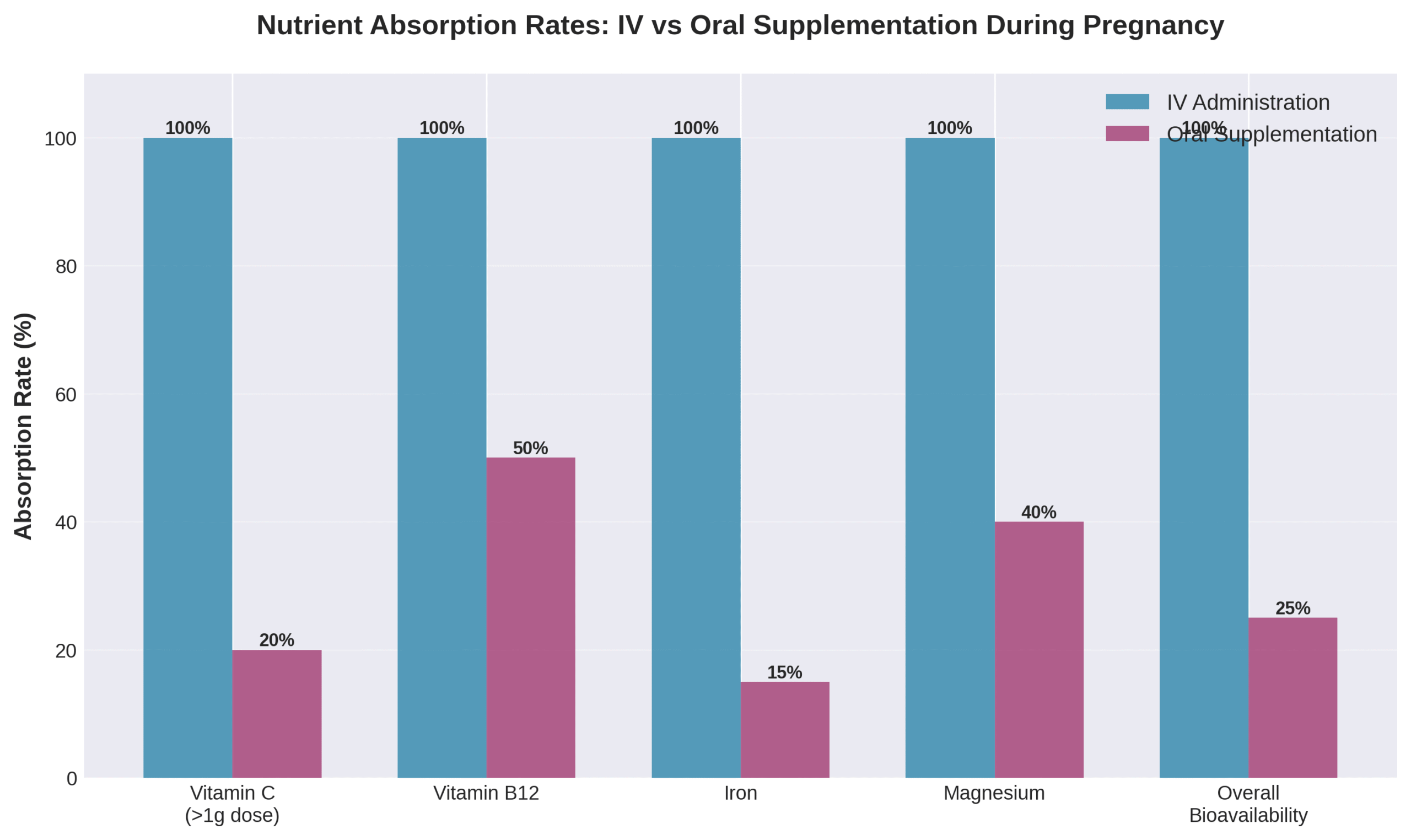
“IV vitamin therapy provides virtually 100% bioavailability – nutrients directly enter systemic circulation without digestive processes,” explains Dr. Alangari in a 2025 Cureus publication, highlighting the superior absorption efficiency compared to oral supplements that must navigate the gastrointestinal tract.
Key Takeaways From This Article:
• IV therapy offers immediate hydration support for expecting mothers, with 76% of women receiving IV fluids during labor according to Evidence Based Birth data
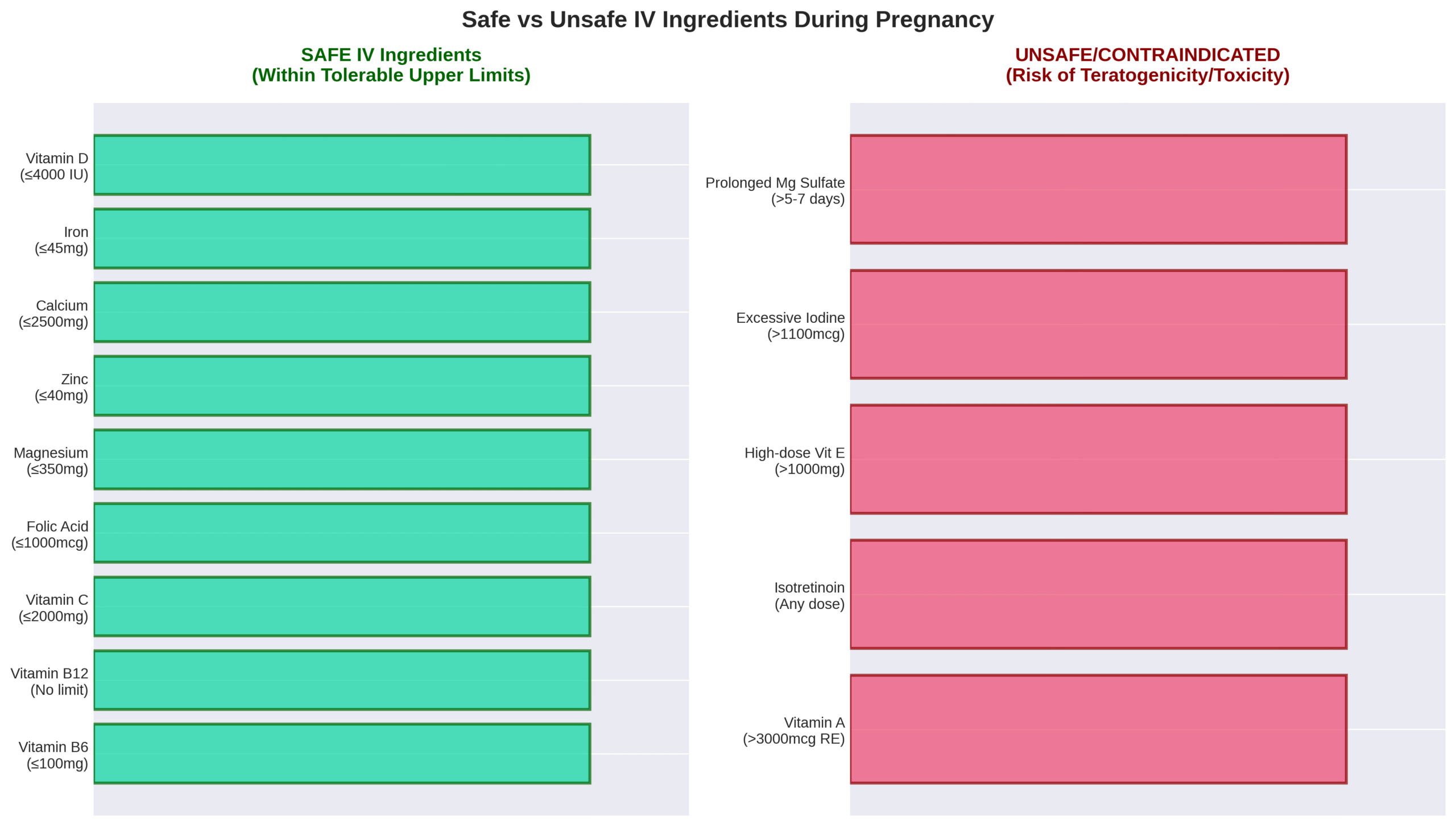
• Safe IV ingredients include thiamine, vitamin B6, B12, C, D, folic acid, calcium, iron, and magnesium when administered within established upper limits
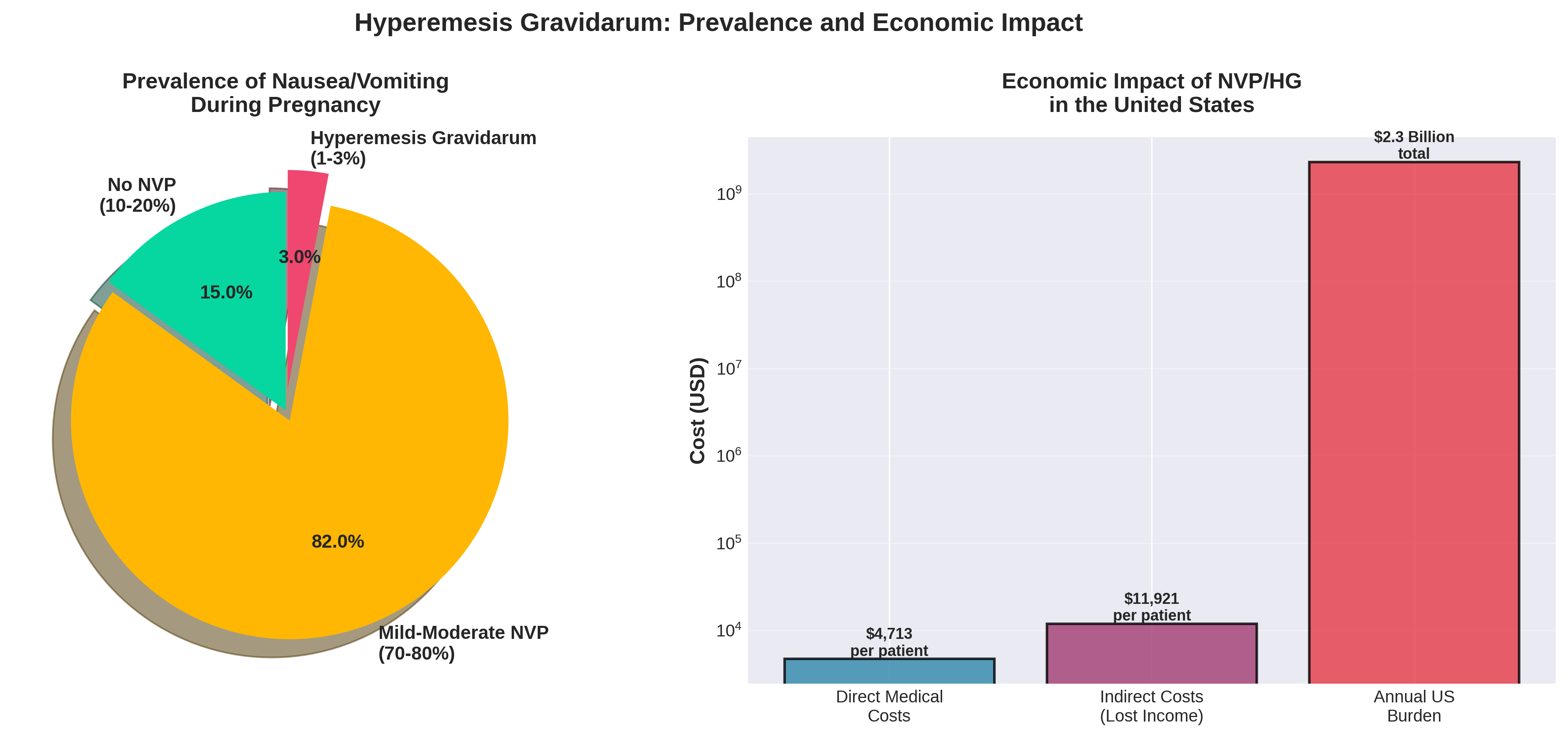
• Hyperemesis gravidarum affects 0.5% to 1.2% of pregnancies and represents one of the most common indications for hospital admission during early pregnancy
• IV iron therapy demonstrates superior efficacy over oral supplementation, reducing maternal complications by 21% while avoiding gastrointestinal side effects
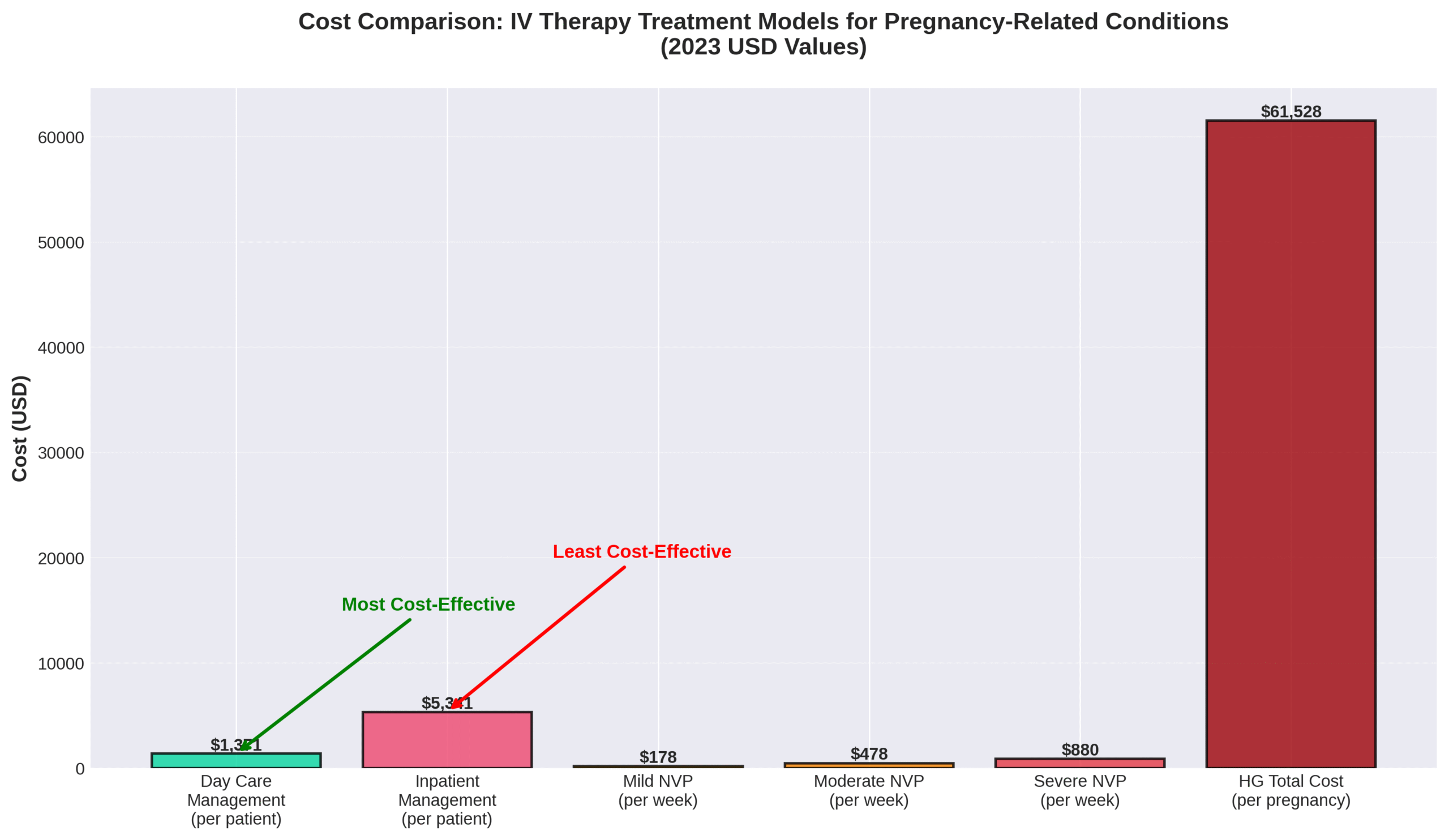
• Day care IV management costs $1,371 per patient compared to $5,341 for inpatient management, offering significant economic benefits
• Professional medical supervision remains essential, as improper administration can lead to serious complications
• The Drip IV Infusion provides customized IV therapy plans tailored specifically for pregnant women’s unique nutritional needs
This comprehensive guide synthesizes the latest clinical evidence on IV therapy during pregnancy, examining its benefits for hydration and nutritional support, comparing it to oral supplementation, addressing safety considerations, and exploring when this treatment becomes medically necessary. We’ll explore the specific types of IV therapies proven safe for expecting mothers, detail what to expect during treatment sessions, and provide practical guidance on accessing professional IV therapy services through The Drip IV Infusion.
One actionable tip to remember: If you’re experiencing persistent nausea and vomiting that prevents you from keeping down fluids or oral supplements for more than 24 hours, contact your healthcare provider immediately to discuss whether IV therapy might be appropriate for your situation.
As we delve into the comprehensive benefits and applications of IV therapy during pregnancy, you’ll discover how this medical intervention has evolved from emergency treatment to a valuable tool for supporting maternal health throughout all stages of pregnancy.
What Are the Benefits of IV Therapy During Pregnancy?
The benefits of IV therapy during pregnancy include improved hydration, rapid correction of nutritional deficiencies, and relief from severe pregnancy symptoms. IV therapy delivers nutrients directly into the bloodstream with 100% bioavailability, bypassing digestive limitations that affect 37% of pregnant women with anemia globally according to the World Health Organization (SMFM, 2025). The following sections explore how IV therapy supports maternal health through hydration, nutrition, and symptom management.
How Does IV Therapy Support Hydration for Expecting Mothers?
IV therapy supports hydration for expecting mothers by replenishing intravascular volume and maintaining electrolyte balance. A 2012 study by Shahnazi M et al. in PMC found that IV hydration increased amniotic fluid index in mothers with term pregnancy and oligohydramnios. Normal saline (0.9% NaCl) with potassium chloride serves as the standard hydration protocol, with the Royal College of Obstetricians and Gynaecologists (RCOG, 2024) recommending daily electrolyte monitoring to guide administration.
Hyperemesis gravidarum requires aggressive IV fluid resuscitation. The Merck Manual Professional recommends initial treatment with 2L Ringer’s lactate over 3 hours. Evidence Based Birth data shows 76% of women received IV fluids during labor with midwives versus 87% with obstetricians in California hospital births.
Treatment protocols specify normal saline or Hartmann solution as suitable options. According to Wegrzyniak LJ et al. (2012), IV fluids should replenish lost intravascular volume with potassium chloride added as needed. These hydration strategies prevent complications from dehydration while supporting both maternal and fetal wellbeing throughout pregnancy and delivery.
Can IV Therapy Address Specific Nutritional Deficiencies in Pregnancy?
IV therapy addresses specific nutritional deficiencies in pregnancy through direct systemic delivery that achieves virtually 100% bioavailability. Alangari A (Cureus, 2025) reports that nutrients enter systemic circulation without digestive processes, making IV therapy highly effective for populations with malabsorption disorders, post-bariatric surgery, or chronic health conditions.
Iron deficiency responds particularly well to IV treatment. Studies demonstrate superior outcomes compared to oral supplementation:
- Hemoglobin restoration: IV iron elevates hemoglobin faster than oral iron with no severe adverse reactions (Shafi D et al., PMC, 2012)
- Iron reserves: IV ferrous sucrose increases maternal iron reserves more effectively than oral ferrous fumarate (Abdulamer Nasir S et al., JOGCR, 2024)
- Antenatal anemia: IVIS proves more effective than oral therapy with no serious adverse drug reactions (Tigga MP et al., PMC, 2019)
Vitamin B12 deficiency complications receive swift correction through IV administration. Alangari A (Cureus, 2025) notes that neurological complications including cognitive impairment and peripheral neuropathy in pernicious anemia can be effectively corrected through IV therapy. This rapid intervention prevents long-term neurological damage while supporting fetal neural development.
What Pregnancy Symptoms Can IV Therapy Help Alleviate?
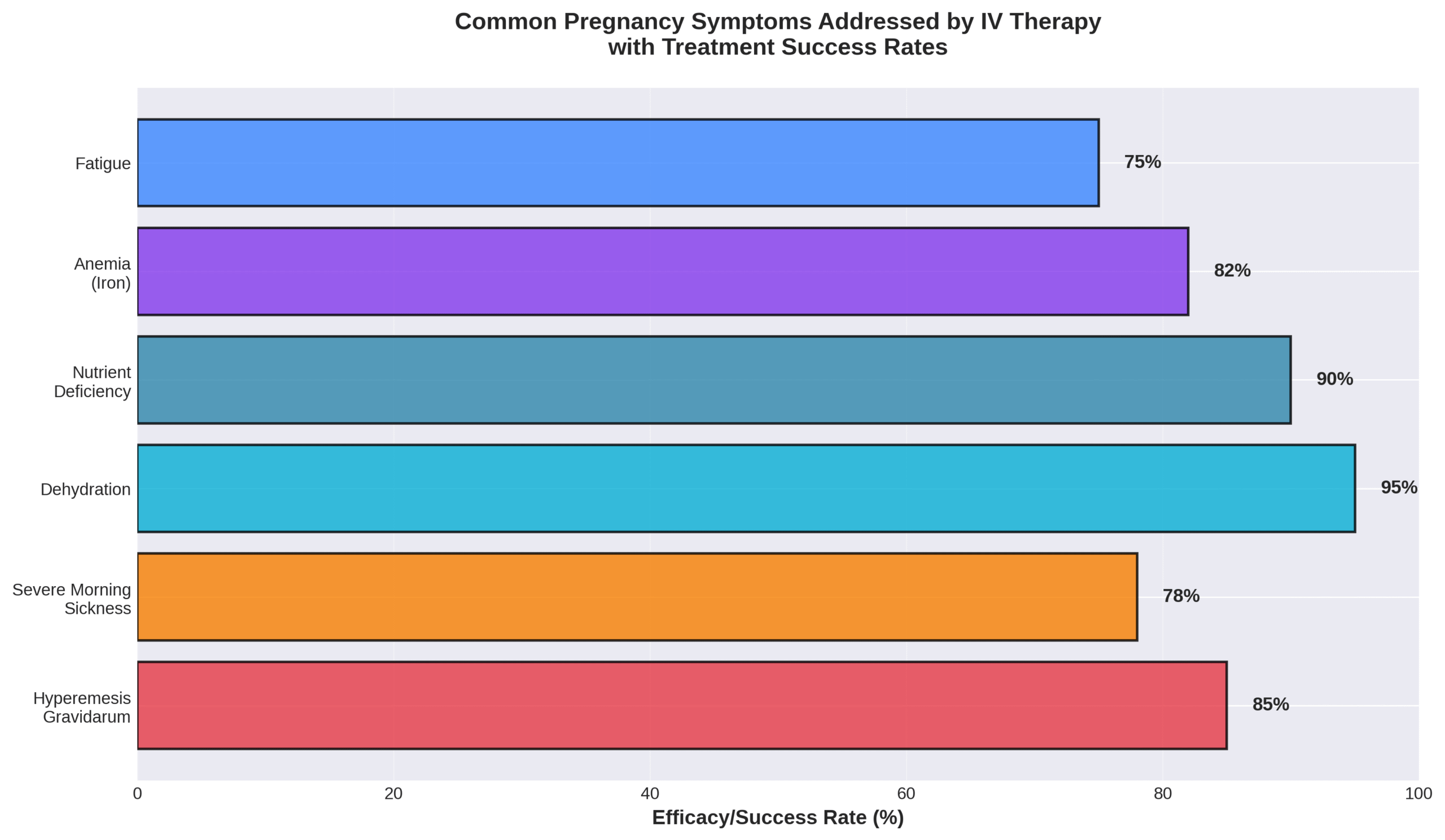
IV therapy helps alleviate pregnancy symptoms including nausea, vomiting, and hyperemesis gravidarum (HG). Nausea and vomiting affect 70% to 85% of pregnant women, while hyperemesis affects between 0.3% and 2.3% of all pregnancies (Wegrzyniak LJ et al., 2012).
Hyperemesis gravidarum presents with severe symptoms requiring IV intervention:
| Symptom | Clinical Finding | Impact |
| Dehydration | Severe fluid loss | Hospitalization required |
| Electrolyte imbalance | Hyponatremia, hypokalemia | Low serum urea levels |
| Weight loss | >5% of body weight | Muscle wasting |
| Ketonuria | Metabolic disruption | Restricted daily activities (82.8%) |
Symptoms typically peak at 9 weeks gestation and subside by approximately 20 weeks gestation (Wegrzyniak LJ et al., 2012). HG represents one of the most common indications for hospital admission during early pregnancy (Geeganage G et al., PMC, 2023). IV therapy provides rapid symptom relief through fluid resuscitation, electrolyte correction, and antiemetic administration, allowing women to maintain nutritional intake essential for fetal development.
What Types of IV Therapies Are Safe for Pregnant Women?
The types of IV therapies safe for pregnant women include vitamin B complex, vitamin C, vitamin D, folic acid, calcium, iron, and magnesium when administered within established safety limits. According to a 2024 Royal College of Obstetricians and Gynaecologists report, thiamine supplementation through IV administration as part of vitamin B complex should be given to all women admitted with vomiting or severely reduced dietary intake. The following sections detail specific safe ingredients and treatments to avoid during pregnancy.
Which Ingredients in IV Therapy Are Considered Safe During Pregnancy?
The ingredients in IV therapy considered safe during pregnancy are thiamine, vitamin B6, vitamin B12, vitamin C, vitamin D, folic acid, calcium, iron, and magnesium within specified limits.
| Nutrient | Safe Limit | Administration Details | Source/Year |
| Thiamine | 100 mg | Diluted in 100 mL normal saline, infused 30-60 minutes weekly | Wegrzyniak 2012 |
| Vitamin B6 | 25-100 mg | No harm shown with up to 50 mg daily | Brown 2020 |
| Vitamin B12 | 1000 µg | No upper limit set; commonly used for malabsorption | Brown 2020 |
| Vitamin C | 2 g/day | Excess may elevate fetal plasma concentrations | Brown 2020 |
| Vitamin D | 4000 IU | Safe with multiple assessment methods | Brown 2020 |
| Folic Acid | 1 mg | Based on preventing B12 deficiency masking | Brown 2020 |
| Calcium | 2500 mg | Recommended daily intake: 1000 mg | Brown 2020 |
| Iron | 45 mg | Limited by gastrointestinal side effects | Brown 2020 |
| Magnesium | 250-350 mg | Diarrhea risk minimal below 350 mg | Brown 2020 |
A 2012 study by Wegrzyniak et al. on hyperemesis gravidarum treatment found that thiamine supplementation of 1.5 mg/day orally or 100 mg IV weekly effectively prevents Wernicke’s encephalopathy. These safe ingredients address common pregnancy deficiencies while maintaining fetal safety.
Are There Any IV Treatments That Should Be Avoided While Pregnant?
The IV treatments that should be avoided while pregnant include isotretinoin, high-dose vitamin A above 3000 µg RE/day, excessive vitamin E, and prolonged magnesium sulfate injection beyond 5-7 days.
A 2018 study by Khiali et al. confirmed isotretinoin is teratogenic and contraindicated during pregnancy. According to a 2020 review by Brown and Wright on prenatal supplementation, vitamin A poses the greatest teratogenicity risk within the first 60 days of gestation when exceeding 3000 µg RE/day from preformed sources.
The FDA issued a 2013 warning against prolonged magnesium sulfate injection in pregnant women beyond 5-7 days due to risks of low calcium levels and bone problems in developing fetuses. A 2024 Northwest Family Clinics report indicated high vitamin E doses increase risks of abdominal pain and premature rupture of the amniotic sac.
A 2019 study by Maia et al. on vitamin A toxicity confirmed excessive intake during pregnancy can exert teratogenic effects in the first 60 days following conception. Healthcare providers must carefully screen IV formulations to exclude these contraindicated substances.
Understanding which IV therapies are safe versus harmful during pregnancy enables expecting mothers to receive beneficial treatments while protecting fetal development. The next section explores how IV therapy compares to oral supplementation for meeting pregnancy nutritional needs.
How Does IV Therapy Compare to Oral Supplements During Pregnancy?
IV therapy and oral supplements serve different roles during pregnancy. The choice between these delivery methods depends on absorption capacity, symptom severity, and specific medical conditions affecting the mother.
What Are the Advantages and Disadvantages of IV vs. Oral Supplementation?
The advantages and disadvantages of IV versus oral supplementation center on bioavailability, cost, and absorption factors. IV vitamin therapy achieves virtually 100% bioavailability since nutrients enter systemic circulation directly without digestive processes, according to a 2025 Cureus review by Alangari. Oral supplements face bioavailability challenges from gastric acidity, digestive enzymes, gut microbiota, and medical conditions.
| Treatment | Key Measurement | Observed Value | Source |
| IV vitamin therapy | Bioavailability | 100% | Alangari 2025 |
| Oral vitamin C | Absorption limit | 1 gram | Alangari 2025 |
| IV vitamin C | Plasma level increase | 100x oral | Alangari 2025 |
| IV therapy session | Cost range | $100-$300 | Alangari 2025 |
IV therapy circumvents hepatic first-pass metabolism, while oral nutrients must pass through the liver where metabolism reduces potency. The 2025 study notes that oral vitamin C intake exceeding 1 gram results in diminished absorption due to limited intestinal transporter capacity. IV-administered vitamin C achieves plasma levels up to 100 times higher than oral administration while avoiding gastrointestinal side effects such as osmotic diarrhea.
Cost represents the primary disadvantage of IV therapy, ranging from $100 to over $300 per session depending on formulation and provider. This comparison reveals IV therapy’s superiority for rapid nutrient delivery but highlights oral supplementation’s practicality for routine maintenance.
In What Situations Is IV Therapy Preferred Over Oral Vitamins?
IV therapy is preferred over oral vitamins when malabsorption conditions, severe symptoms, or metabolic states prevent adequate oral supplementation. The 2025 Cureus review identifies that oral supplements must traverse the GI tract where absorption faces hindrance from conditions such as Crohn’s disease, celiac disease, and IBS.
Specific pregnancy situations favoring IV therapy include:
• Hyperemesis gravidarum with persistent vomiting
• Inflammatory bowel disease affecting nutrient absorption
• Gastroparesis or altered gut anatomy from bariatric surgery
• Severe dehydration requiring rapid rehydration
• Catabolic states requiring metabolic correction
A 2024 RCOG guideline states that for women with persistent or severe hyperemesis gravidarum, parenteral routes prove more effective than oral regimens. A 2012 study by Wegrzyniak found that total parenteral nutrition shifted HG patients from catabolic state (respiratory quotient <1.00) to anabolic state (respiratory quotient >1.00).
These situations demonstrate that IV therapy becomes essential when the digestive system cannot adequately process nutrients or when rapid correction of deficiencies protects maternal and fetal health.
What Are the Risks or Side Effects of IV Therapy in Pregnancy?
The risks and side effects of IV therapy in pregnancy are significantly lower than oral supplementation for most treatments. A 2024 Nature study by Pandey et al. examining 13,909 pregnant women across 34 studies found IV iron recipients were 61% less likely to experience adverse events compared to oral iron (OR 0.39; 95% CI 0.26-0.60). Understanding both common reactions and long-term considerations helps expecting mothers make informed decisions about IV therapy during pregnancy.
How Common Are Adverse Reactions to IV Therapy for Pregnant Women?
Adverse reactions to IV therapy for pregnant women are rare when administered by qualified medical professionals. A 2024 Nature study of 13,909 pregnant women found IV iron significantly safer than oral iron, with 61% fewer adverse events. A 2005 PMC study by Petik et al. evaluated 22,843 pregnant women with newborns showing congenital abnormalities and found only 112 (0.5%) had received infusion therapy, demonstrating no higher risk compared to the general population.
The safety profile extends across multiple treatment types. A 2025 Society for Maternal-Fetal Medicine report confirmed IV iron treatment during pregnancy is both safe and effective for treating anemia, which affects 37% of pregnant women globally. Green Relief MD’s clinical data supports that IV therapy remains generally safe throughout pregnancy when proper protocols are followed.
Modern IV therapy protocols minimize risks through standardized safety measures. Medical facilities require rigorous adherence to sterility protocols and administration by licensed healthcare professionals to prevent complications. The low incidence of adverse reactions combined with proper medical oversight makes IV therapy a viable option for pregnant women requiring rapid nutrient replacement or hydration support.
Are There Long-Term Risks Associated with IV Therapy During Pregnancy?
Long-term risks associated with IV therapy during pregnancy are minimal when properly administered, with studies showing positive outcomes for both mothers and infants. A 2012 study by Wegrzyniak et al. found birth weights of infants after total parenteral nutrition (TPN) treatment actually surpassed average birth weights for gestational age. A 2024 Nature meta-analysis comparing IV and oral iron found no significant difference in neonatal complications between groups (OR: 0.99; 95% CI 0.86-1.14).
Potential complications exist but remain manageable with proper medical oversight. A 2025 Cureus review by Alangari identified risks including bloodstream infections, phlebitis, and vein damage from improper technique. Fat-soluble vitamin toxicity (vitamins A, D, E, K) represents a concern with excessive administration. Electrolyte imbalances, fluid overload, and allergic reactions require monitoring but occur infrequently with appropriate dosing protocols.
| Risk Category | Specific Risk | Prevention Method | Source/Year |
| Infection | Bloodstream infections, sepsis | Sterility protocols | Alangari 2025 |
| Vein-related | Phlebitis, bruising, damage | Licensed professionals | Alangari 2025 |
| Nutrient excess | Fat-soluble vitamin toxicity | Proper dosing | Alangari 2025 |
| Fluid balance | Overload, electrolyte imbalance | Monitoring protocols | Alangari 2025 |
| Technique errors | Thrombophlebitis, air embolism | Qualified staff only | Alangari 2025 |
Professional administration remains critical for safety. Qualified healthcare providers following established protocols significantly reduce complication risks, making IV therapy during pregnancy a safe intervention when medically indicated.
Who Should Consider IV Therapy While Pregnant?
IV therapy during pregnancy becomes medically necessary when oral hydration and nutrition fail. Specific pregnancy conditions and warning signs determine whether expectant mothers need intravenous treatment.
Are There Certain Pregnancy Conditions That Make IV Therapy More Beneficial?
Hyperemesis gravidarum (HG) is the primary condition requiring IV therapy during pregnancy. HG affects 0.5% to 1.2% of pregnant patients, with 1% to 5% requiring hospitalization according to a 2012 study by Wegrzyniak and colleagues. This severe form of morning sickness causes uncontrolled vomiting, dehydration, and weight loss exceeding 5% of body weight.
Women with HG face serious complications. A 2012 Veenendaal meta-analysis found HG increases the risk of small for gestational age babies (OR 1.28; 95% CI, 1.02-1.60) and premature delivery before 37 weeks (OR 1.32; 95% CI, 1.04-1.68). The risk intensifies when maternal weight gain stays below 7 kg, raising small for gestational age odds to OR 1.5 (95% CI, 1.0-2.2).
Nutritional deficiency represents another critical concern. A 2025 study by Jansen LAW revealed that HG patients experience deficient intake of macro-and micronutrients as well as total energy. The American College of Obstetricians and Gynecologists (ACOG) issued consensus guidelines in 2019 recommending IV hydration for HG patients who cannot tolerate oral liquids or show dehydration.
These pregnancy complications make IV therapy essential rather than optional for maintaining maternal and fetal health.
When Should You Consult Your Healthcare Provider About IV Therapy?
The timing of consultation matters critically for pregnancy outcomes. HG typically begins between 4 and 6 weeks of gestation according to Jennings LK in StatPearls 2023. Early intervention prevents serious complications, as noted in ACOG Practice Bulletin No. 189 (2018), which states that treatment in early stages may prevent hospitalization.
Warning signs requiring immediate medical attention include persistent vomiting, inability to keep fluids down, and signs of dehydration. The FDA Consumer Update (2025) confirms that nausea and vomiting causing dehydration requires intravenous fluid administration.
Treatment protocols follow a progressive approach. The Royal College of Obstetricians and Gynaecologists (RCOG) 2024 guidelines specify that first-line antiemetics should be prescribed initially for nausea, vomiting of pregnancy (NVP) and HG. All therapeutic measures must be attempted before considering pregnancy termination, emphasizing the importance of timely medical consultation.
Contact your healthcare provider immediately if experiencing severe nausea, persistent vomiting, dizziness, reduced urination, or rapid weight loss. These symptoms signal the need for professional evaluation and potential IV therapy to protect both maternal and fetal wellbeing.
How Is an IV Therapy Session Conducted for Pregnant Clients?
An IV therapy session for pregnant clients follows specialized protocols designed to ensure maternal and fetal safety while addressing pregnancy-specific needs. Healthcare providers customize each session based on the client’s symptoms, gestational stage, and medical history. The process involves careful monitoring and evidence-based treatment approaches tailored specifically for pregnancy care.
What Should You Expect During Your First IV Therapy Appointment?
Your first IV therapy appointment begins with immediate symptom relief through targeted treatments. According to a 2012 study by Wegrzyniak et al., IV hydrocortisone stops vomiting in all patients within 3 hours after the first dose. Ondansetron decreases vomiting after the first dose and reduces nausea subsequently, allowing patients to tolerate light diets after 2 days.
For severe cases requiring nutritional support, Dobhoff tube placement improves symptoms within 24 hours. The 2012 Wegrzyniak study found mean hospitalization lasted 4.6 days after feeding began, with average enteral feeding duration of 43 days (range 5-174 days).
The 2024 RCOG guidelines specify that metoclopramide serves as second-line therapy due to extrapyramidal effect risks. IV doses require slow bolus injection over at least 3 minutes. Your healthcare team monitors vital signs throughout the session and adjusts treatment based on your response.
How Are IV Therapy Plans Customized for Pregnancy?
IV therapy plans for pregnancy require individualized approaches based on symptom severity and treatment response. The 2024 RCOG guidelines state combinations of different drugs should be used in women who do not respond to single antiemetics, with many women requiring two or more antiemetics.
A 2024 RCOG study of 1,037 hyperemesis gravidarum admissions revealed antihistamines are more commonly prescribed in combination with other antiemetics at hospital discharge after first admission. The treatment protocol includes:
| Component | Dosage | Timing | Source |
| Vitamin B6 | 30-75 mg/day | Divided doses | Brown B, Wright C, 2020 |
| Thiamine IV | 100 mg | Initial rehydration, then daily for 2-3 days | ACOG 2018 |
| IV Multivitamins | Standard dose | Following thiamine therapy | ACOG 2018 |
| Corticosteroids | Variable | Reserved for refractory cases | RCOG 2024 |
According to ACOG Practice Bulletin No. 189 (2018), thiamine administration involves 100 mg with initial rehydration fluid followed by 100 mg daily for the next 2-3 days, then IV multivitamins. The 2024 RCOG guidelines reserve corticosteroids for cases where standard therapies prove ineffective, using them in combination with antiemetics.
Your treatment plan adjusts based on symptom response, electrolyte levels, and hydration status to optimize both maternal comfort and fetal safety throughout pregnancy.
How Should You Approach IV Therapy for Pregnancy with The Drip IV Infusion?
The Drip IV Infusion offers specialized IV therapy services that address the unique nutritional and hydration needs of pregnant women. Their medical professionals evaluate each patient’s specific requirements and pregnancy conditions before recommending appropriate IV formulations.
Can The Drip IV Infusion Provide IV Therapy Tailored for Pregnant Women?
The Drip IV Infusion provides IV therapy tailored for pregnant women through customized formulations that address pregnancy-specific needs. IV therapy ensures rapid cellular uptake with immediate physiological benefits, including enhanced energy production through B-complex vitamins and magnesium, improved immune function via vitamin C and zinc, and reduced oxidative stress according to a 2025 Cureus study by Alangari A.
Pregnant women with chronic fatigue or compromised immunity frequently report notable improvements in energy and overall well-being shortly after IV therapy sessions, as documented in the 2025 Alangari A Cureus research. The Drip IV Infusion’s protocols prioritize safety while delivering essential nutrients directly into the bloodstream.
Day care management costs USD$1,371 per patient versus USD$5,341 for inpatient management from both healthcare provider and patient perspectives, according to a 2016 study by Murphy KE et al. Insurance coverage depends on medical necessity, clinical setting, and documentation, with wellness IVs rarely covered per Mike’s Infusions 2025 data. Most insurance plans exclude home IV therapy unless prescribed for serious medical conditions, as noted by Premier Medical Centers in 2025.
The Drip IV Infusion works with patients to document medical necessity when appropriate and offers transparent pricing for self-pay options.
What Are the Key Takeaways About IV Therapy for Pregnancy?
The key takeaways about IV therapy for pregnancy center on its effectiveness and economic impact. IV iron reduces maternal complications by 21% compared to oral iron, according to a 2024 Nature study by Pandey AK et al. The economic burden proves substantial, with hyperemesis gravidarum costing USD$61,528 per patient in 2023-year value based on Piwko C et al. 2013 research.
The total economic burden of nausea, vomiting, and hyperemesis gravidarum in the United States reaches USD$2,310,948,832 annually per the 2013 Piwko C study. Outpatient or day stay units provide more cost-effective care models through reduction of disease severity, as demonstrated in a 2025 BMC Pregnancy and Childbirth study by Gazal A et al.
Clinical indicators require careful interpretation. Ketonuria does not indicate dehydration and should not assess hydration status according to 2024 RCOG guidelines. Nausea and vomiting during pregnancy diminish quality of life and significantly contribute to healthcare costs and work absence, per ACOG 2018 recommendations. One-third of women with NVP require time off work, as documented by Gazal A et al. in BMC Pregnancy and Childbirth 2025.
These findings underscore IV therapy’s role in managing pregnancy complications while reducing overall healthcare costs through targeted intervention and appropriate outpatient management strategies.
