IV therapy is covered by insurance only when it is medically necessary for diagnosed conditions; elective vitamin IV infusions are not covered. If you’re wondering whether your insurance will cover IV therapy or vitamin IV infusions, you’ve come to the right place. We get it—figuring out insurance coverage for these treatments can feel like solving a puzzle, especially when you’re trying to tell the difference between medical IV therapy and wellness infusions. Think of us as your guide through this maze of insurance rules, helping you understand what you can expect when it comes to paying for these treatments.
IV therapy is when healthcare providers give you fluids, medications, and nutrients straight into your bloodstream through a small tube in your vein. It’s like getting nutrients delivered directly to your body’s doorstep instead of having them go through the long route of your digestive system first—that’s why it works so much better than taking pills.
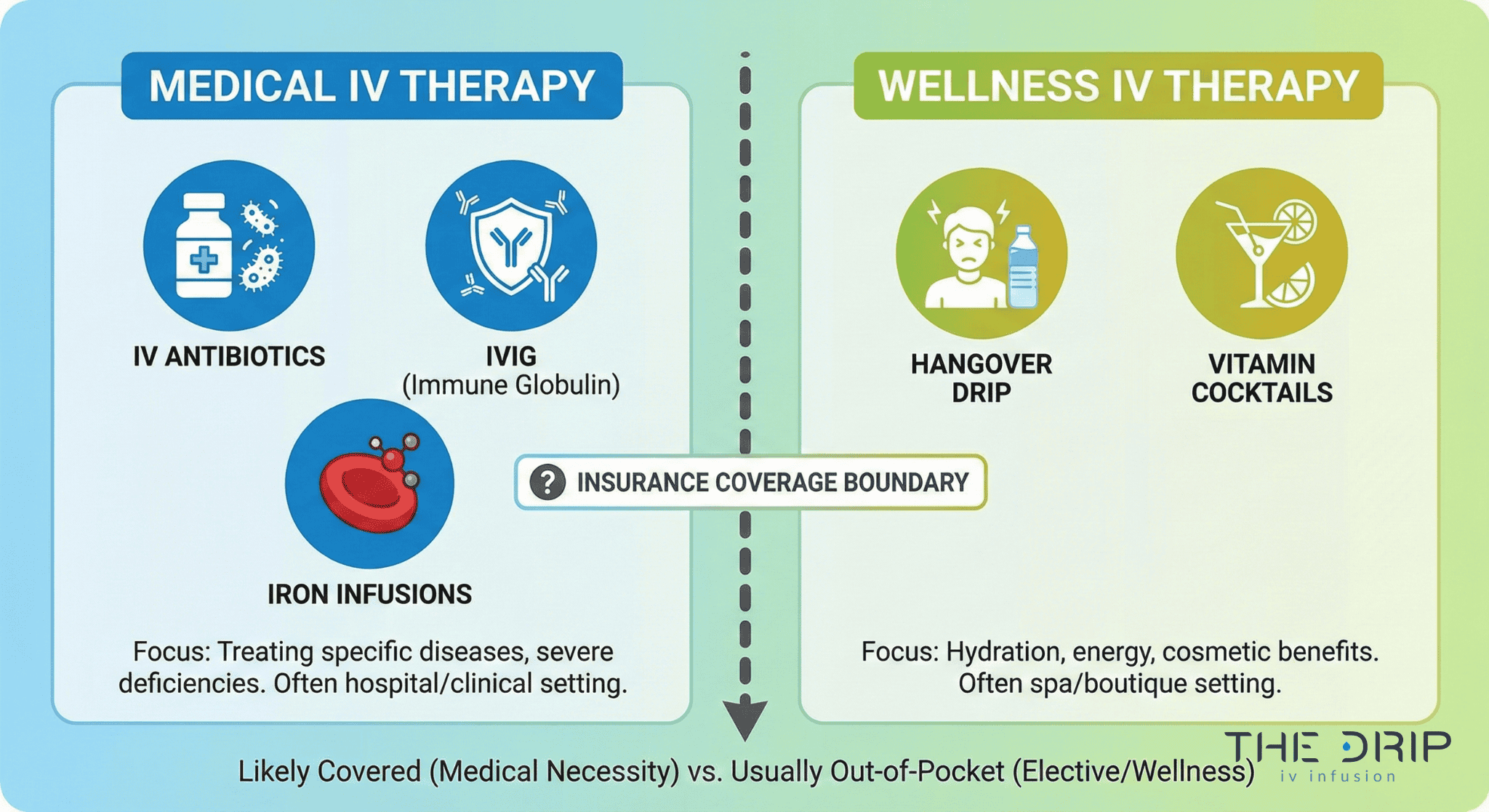
Your insurance company looks at IV therapy in two completely different ways: the kind doctors prescribe to treat real medical problems (like special antibodies for autoimmune diseases or IV antibiotics for serious infections), which insurance usually pays for, and the wellness kind for general health (like hangover cures or vitamin cocktails), which insurance almost never covers. This difference between medical treatment and wellness service is what decides whether you’ll be reaching for your wallet or not.
TL;DR Summary:
• Insurance covers IV therapy when it’s medically necessary for diagnosed conditions with proper documentation, but excludes elective vitamin IV therapy for wellness purposes
• Coverage varies significantly by insurance type (HMO, PPO, Medicare) with HMOs requiring in-network providers and referrals while PPOs offer more flexibility
• Medical conditions qualifying for coverage include immunodeficiencies, autoimmune disorders, severe anemia, dehydration from diagnosed conditions, serious infections, and documented nutritional deficiencies
• Insurance companies universally exclude wellness IV therapy like hangover drips, energy boosters, and beauty treatments as not medically necessary
• Prior authorization can take 1 day to 1 month with 96% eventual approval rate, though 82% of initial denials are overturned on appeal
• Out-of-pocket costs range from $100-500 per session for wellness IV therapy to over $9,720 per infusion for medical treatments like IVIG
• Alternative payment options include HSA/FSA funds (with physician prescription), manufacturer assistance programs, and payment plans from providersQuick Tip: Before you schedule any IV therapy, call your insurance company with the specific billing codes (96360-96361 for hydration, 96365-96366 for therapeutic infusion) to check what’s covered and what you’ll pay out of pocket. This one phone call can save you from a nasty surprise when the bill arrives—we’re talking thousands of dollars in some cases.
What is IV therapy and how does vitamin IV therapy differ?
IV therapy is the medical process of delivering fluids, medications, and nutrients directly into the bloodstream, and it differs from vitamin IV therapy because insurers classify one as medically necessary treatment and the other as elective wellness care. The medical kind includes treatments like IVIG for autoimmune disorders, biologic infusions for Crohn’s disease, and IV antibiotics for serious infections. The wellness kind covers things like hangover relief drips, athletic performance infusions, and anti-aging vitamin cocktails.
How does IV therapy work?
IV therapy works by skipping your digestive system entirely and putting substances directly into your blood circulation. Your healthcare provider puts a small catheter (that’s medical talk for a tiny tube) into a vein, usually in your arm or hand. The IV solution flows from a bag through tubing right into your bloodstream at a steady, controlled pace. This direct delivery method means your body gets everything immediately and completely. Most vitamin infusions take about 30 to 60 minutes to finish.
What are the typical uses of vitamin IV therapy?
People typically use vitamin IV therapy for immune support, energy boosts, and beauty treatments, though the scientific evidence backing these benefits is pretty thin. A 2009 study looked at something called Myers’ Cocktail for fibromyalgia and found some positive results, but the study was small and the placebo effect was pretty high. IV vitamin C has been studied for helping cancer patients feel better, but the FDA hasn’t approved it as a cancer treatment. Common reasons people seek it out include hydration, getting nutrients back up, and general wellness optimization.
Why do people seek out vitamin IV therapy?
People go for vitamin IV therapy because they think it’ll give them quick wellness benefits and it’s convenient. The North American IV hydration therapy market was worth $1.6 billion in 2024 and is expected to grow by 8.7% each year through 2030. But here’s the thing—according to Mayo Clinic’s Dr. Brent A. Bauer, there’s limited evidence that IV vitamins help people who already eat well and get good nutrition. People are motivated by wanting relief from fatigue, faster recovery from workouts, and immune system boosts, even though the science to back this up is minimal.
Understanding these differences helps you figure out whether your IV therapy needs will match up with what insurance covers or if you’ll be paying out of your own pocket.
Which types of health insurance typically cover medical IV therapy?
The types of health insurance that usually cover medical IV therapy are HMO plans, PPO plans, and Medicare. HMO plans will only cover IV therapy if you go to doctors in their network and get a referral from your primary care doctor first—they won’t pay for out-of-network treatment except in emergencies. PPO plans give you more freedom, covering both in-network and out-of-network IV therapy, but going out-of-network will cost you a lot more out of pocket. Medicare Part B covers medically necessary outpatient IV therapy, while Part D covers the medications used in home infusions. Insurance companies like Aetna have strict rules about cost-effectiveness—they’ll only cover IV therapy if it doesn’t cost more than other treatments that work just as well. Knowing what type of plan you have determines both where you can go for treatment and how much you’ll pay.
When is IV therapy considered medically necessary for insurance?
IV therapy is considered medically necessary when doctors prescribe it to diagnose, treat, or cure documented medical problems. Insurance companies need a formal diagnosis with the right medical code and complete supporting medical records before they’ll approve coverage. The treatment has to address a specific medical need, not just general wellness or prevention. Aetna’s policy for intravenous iron therapy shows how strict these requirements are—they specify exact diagnostic criteria like having serum ferritin levels below 30 ng/mL and transferrin saturation below 20%. Medical necessity decisions involve clinical documentation proving that getting the treatment through an IV is essential because pills either didn’t work or can’t be used for some medical reason.
Which diagnoses make IV therapy likely to be covered?
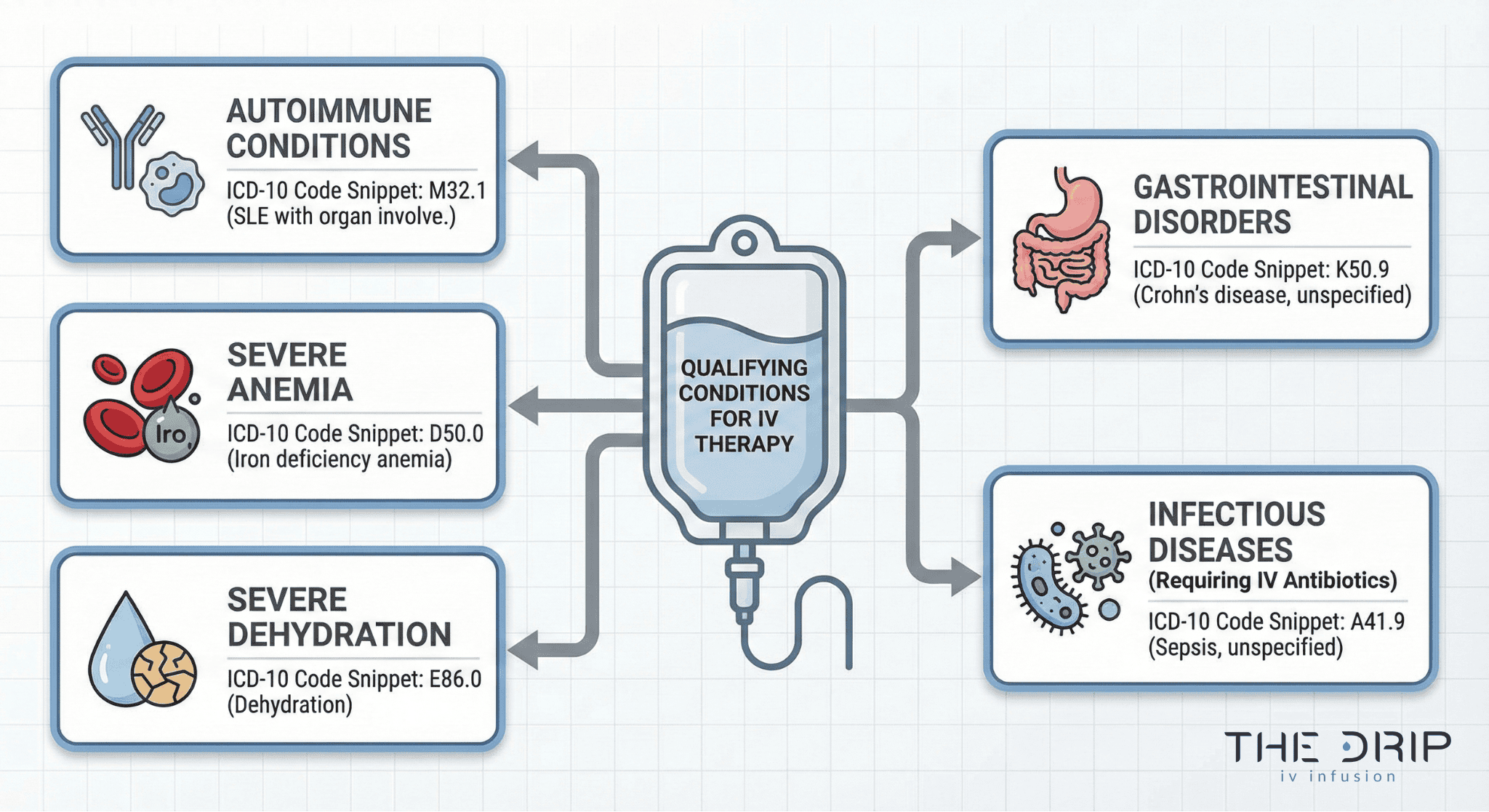
These diagnoses fall into predictable categories, and breaking them into a list makes clinical patterns easier to understand.
| Condition Category | Diagnosis Description | ICD-10 Codes |
| Immune Disorders | Primary immune deficiencies | D80.0, D80.1 |
| Immunodeficiency | Common variable immunodeficiency | D83.9 |
| Autoimmune | Crohn’s, RA, MS | K50.9, M06.9, G35 |
| Anemia | Iron-deficiency anemia | D50.9 |
| Dehydration | Hypovolemia/Dehydration | E86.0, E86.1 |
| Infections | Endocarditis, Osteomyelitis | I33.0, M86.9 |
| Malabsorption | Nutrient absorption disorders | K90.9 |
| Surgical Complications | Post-bariatric absorption problems | Z98.84 |
Does insurance differentiate between in-hospital and outpatient IV therapy?
Yes. Insurance differentiates between in-hospital and outpatient IV therapy, applying different coverage rules and payment structures. Insurance treats in-hospital and outpatient IV therapy differently when it comes to coverage and how much they pay. Home infusion gets strong encouragement from insurance companies because it cuts costs by 30 to 60% compared to hospital settings while working just as well. The location where you get treatment significantly affects both whether it’s covered and how the billing works—outpatient facilities use different billing codes than hospital-based infusion centers. Medicare shows this difference clearly by splitting home infusion coverage between Part B for equipment rental and professional services and Part D for the actual medications you receive. Insurance companies encourage outpatient and home-based IV therapy by charging you lower copayments and giving you access to more providers, recognizing that these settings provide the same care for less money.
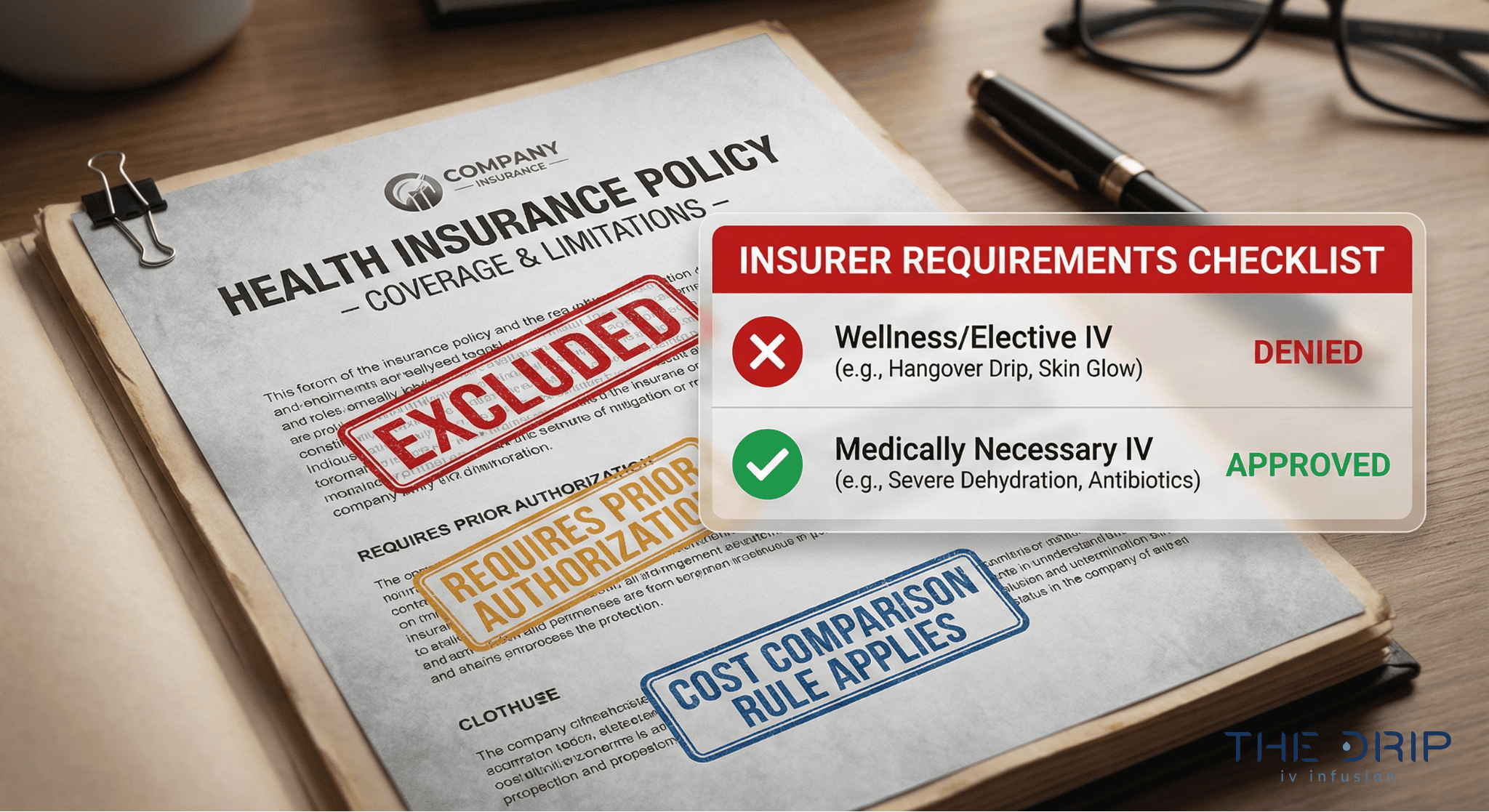
Is vitamin IV therapy regarded as medically necessary by insurance providers?
Insurance companies classify IV therapy based on medical necessity criteria. This table shows how they differentiate medical vs wellness infusions.
| IV Therapy Type | Medical Status | Coverage |
| IV antibiotics | Medically necessary | Covered |
| IVIG | Medically necessary | Covered |
| Iron infusions | Medically necessary | Covered |
| Vitamin drips | Not medically necessary | Not covered |
| Hangover/beauty/energy drips | Elective | Not covered |
The following sections explore specific exceptions and what kind of paperwork insurers demand for vitamin IV therapy claims.
Are there exceptions when vitamin IV therapy might be covered?
Vitamin B12 deficiency (E53.8) with documented absorption problems might qualify for coverage. Nutritional deficiencies from diagnosed absorption disorders like celiac disease may get approved when oral supplements don’t work. Patients after surgery with documented inability to absorb oral vitamins may qualify for coverage under specific medical codes.
Insurance companies look at each case individually based on medical documentation showing that IV administration is the only treatment option that will work. Coverage exceptions require both a qualifying diagnosis and proof that standard oral supplements have failed or can’t be used because of the patient’s specific medical condition.
What evidence do insurers require for vitamin IV therapy claims?
A Letter of Medical Necessity from the prescribing doctor is typically required for vitamin IV therapy claims. Documentation must show that oral supplements have failed or can’t be used due to absorption problems, severe deficiency, or physical issues. Lab results confirming specific vitamin deficiencies must be provided, including baseline levels and follow-up testing.
Insurers demand comprehensive medical records including test results, treatment history, and clinical notes supporting IV administration over oral alternatives. Prior authorization submissions must include billing codes 96365-96366 for therapeutic infusion along with corresponding product codes for specific vitamin formulations. The paperwork burden often discourages providers from pursuing coverage for borderline cases.
What are common reasons insurance denies coverage for IV or vitamin IV therapy?
Common reasons insurance denies coverage for IV or vitamin IV therapy include paperwork mistakes, arbitrary medical thresholds, and misclassifying FDA-approved treatments. A 2023 study shows that 82% of initial denials eventually get overturned, often because of administrative errors. Insurance companies often set arbitrary medical thresholds and misclassify FDA-approved drugs to block expensive treatments.
Blue Cross Blue Shield shows how inconsistent coverage decisions can be through documented cases. Blue Cross Blue Shield of Illinois approved, denied, retroactively approved, then denied again IVIG infusions costing $13,000 per session. Blue Cross of Idaho denied FDA-approved antibody therapy by claiming it was “experimental” despite having FDA approval.
The following sections look at specific exclusion categories and policy definitions that lead to coverage denials.
Is wellness or elective IV therapy usually excluded?
Yes. Wellness or elective IV therapy is always excluded from insurance coverage. Insurance companies exclude hangover recovery drips, energy boost infusions, and beauty vitamin cocktails without any exceptions. General wellness hydration without a medical diagnosis receives no coverage from any major insurer. Athletic performance enhancement IV therapy falls under elective treatment categories and stays excluded from all standard health insurance plans.
These exclusions apply no matter how qualified your provider is or what type of facility you go to. Insurance policies explicitly put wellness IV therapy in the cosmetic or lifestyle enhancement category rather than medical treatment.
How do insurance policies define “alternative” or “complementary” therapies?
Insurance policies define “alternative” or “complementary” therapies through bundling rules and cost-comparison criteria. UnitedHealthcare bundles evaluation and management services as inherent components that can’t be billed separately, preventing additional billing for complementary services. Aetna policies exclude treatments that cost more than alternatives with the same results, establishing cost-effectiveness as a coverage criterion.
These definitions create coverage barriers even for doctor-prescribed treatments. Insurers apply these classifications to deny coverage for vitamin IV therapy despite potential therapeutic benefits in specific cases.
How can you verify if your insurance plan will cover IV therapy?
Verifying insurance coverage for IV therapy requires talking directly with your provider and understanding how long approvals take. The prior authorization process takes anywhere from one day to one month for approval. Healthcare providers spend nearly two business days weekly managing prior authorizations. While 96% of prior authorization requests eventually get approved, the median treatment delay after denial reaches 50 days. Financial assistance programs help 30% of AmeriPharma patients pay nothing out-of-pocket.
Which questions should you ask your insurance provider?
The questions you should ask your insurance provider focus on specific billing codes and coverage details.
| Service Type | Code Type | Codes |
| Hydration | CPT | 96360–96361 |
| Therapeutic infusion | CPT | 96365–96366 |
| IV push | CPT | 96374–96375 |
| IVIG medications | HCPCS | J1459, J1561, J1566, J1568, J1569, J1572 |
Determine your copay and coinsurance amounts for each service type.
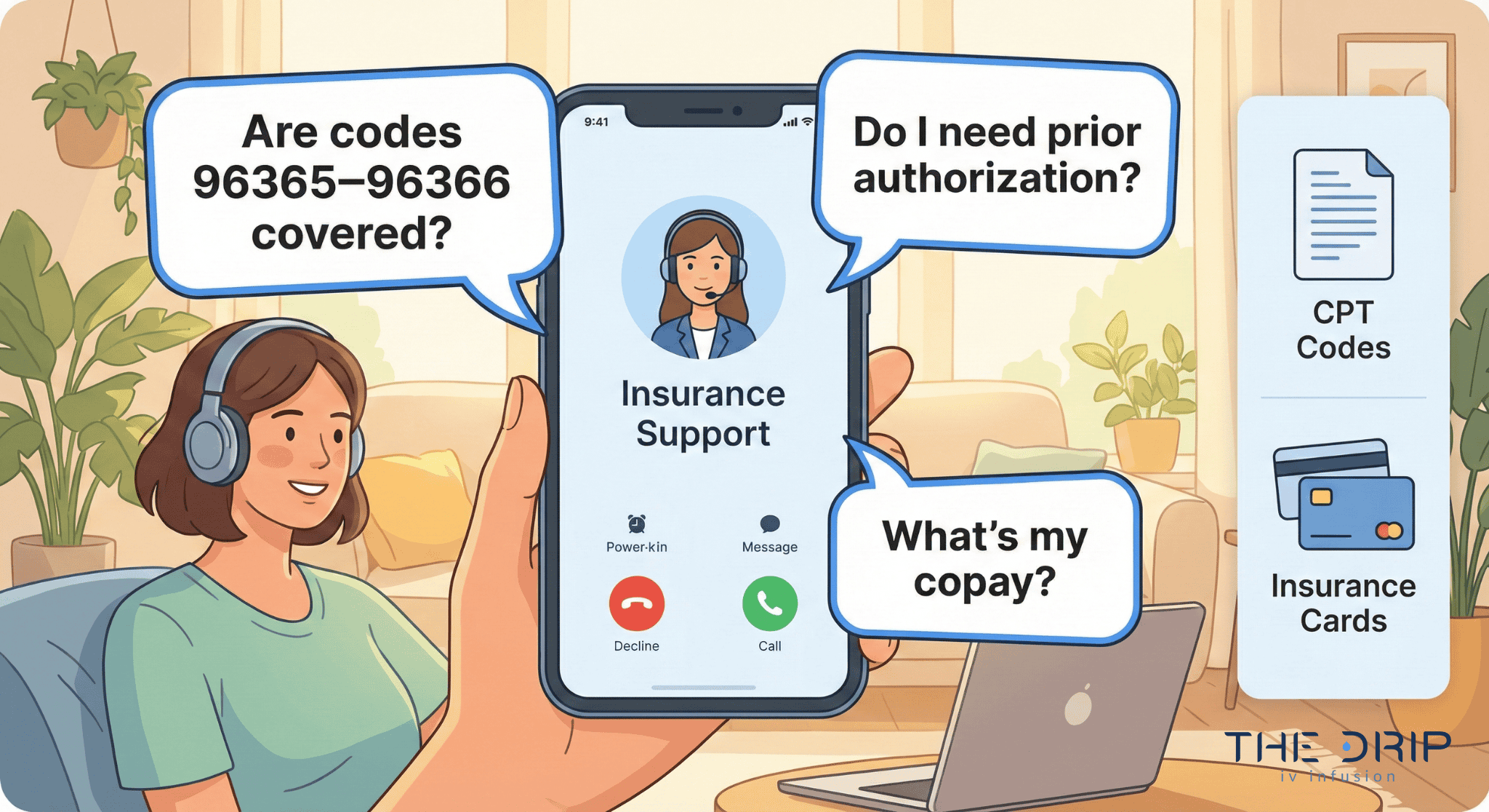
What documentation or referrals may insurance require?
The documentation insurance requires mandatory doctor’s prescriptions with medical diagnosis codes for coverage consideration. HMO plans require referrals from your primary care doctor before you can get specialist IV therapy treatment. Prior authorization paperwork must include medical records supporting clinical necessity. Insurance companies review these documents to confirm the treatment meets medical necessity criteria established in their coverage policies.
Understanding these verification steps helps you navigate insurance requirements efficiently while preparing for potential out-of-pocket costs if coverage gets denied.
Are there alternative ways to pay for IV or vitamin IV therapy if not covered?
This section contains multiple cost ranges and drug examples that scan better as organized bullet points.
- IVIG costs $100–$350 per gram
- Average infusion: $9,720
- Tepezza: $16,000 per treatment
- Monthly IVIG courses exceed $41,000
- Wellness IV therapy: $100–$500 per session
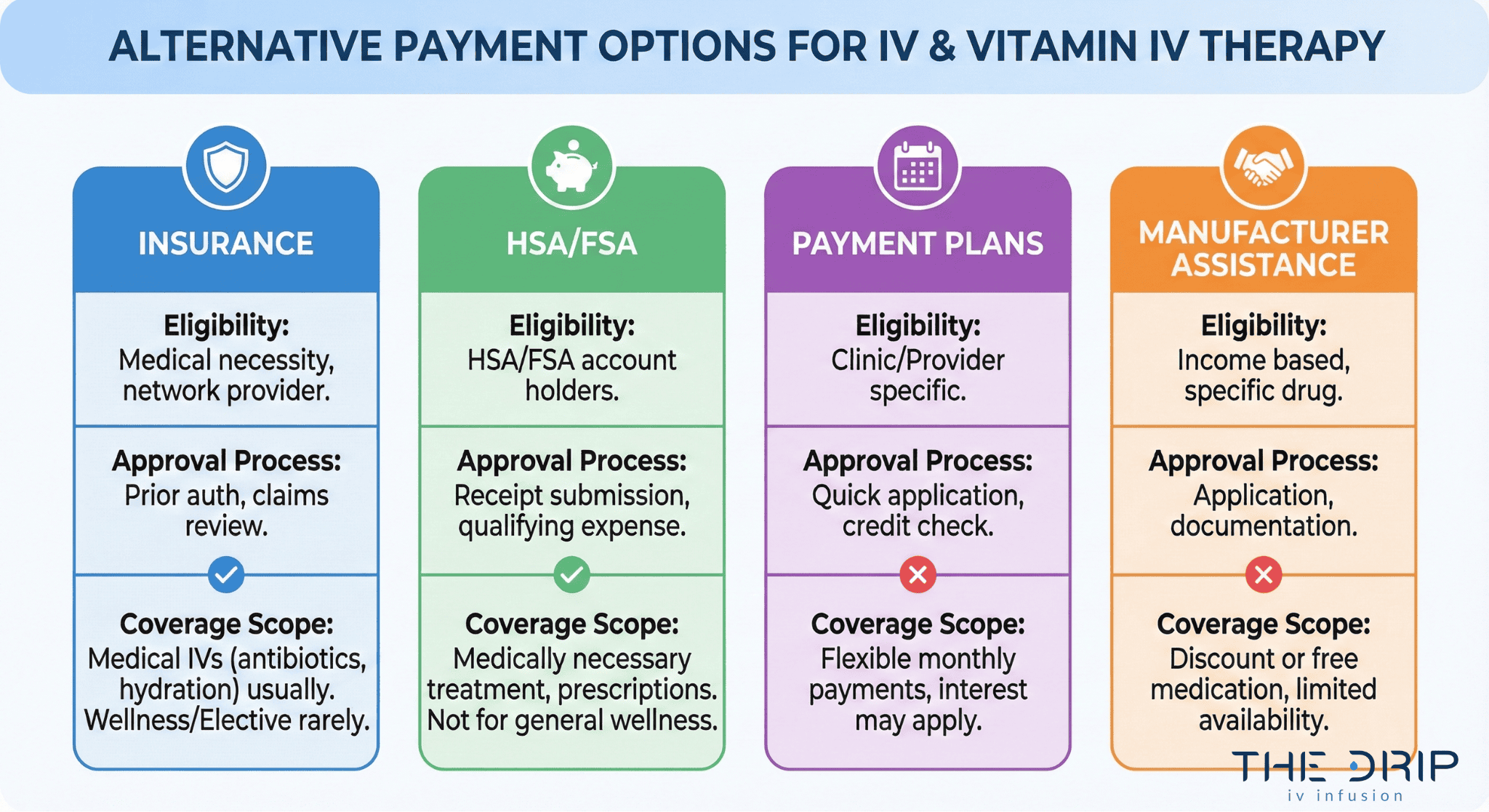
Can you use health savings accounts (HSA) or flexible spending accounts (FSA)?
Yes. You can use HSA or FSA funds for medically necessary IV therapy prescribed by a doctor. The IRS requires a Letter of Medical Necessity for HSA/FSA reimbursement of IV therapy. Qualified medical expenses include IV treatments for diagnosed conditions like dehydration, nutrient deficiencies, or chronic illnesses. Elective wellness-focused IV therapy stays ineligible for HSA/FSA reimbursement. Tax-advantaged accounts provide significant savings for medically necessary infusions when insurance denies coverage.
Are payment plans or package discounts available from providers?
Yes. Many providers offer payment plans, package discounts, and financial assistance options. Payment assistance programs are available through several channels.Clear types of assistance can be broken out for easier comparison:
- Manufacturer copay programs
- Charitable foundations
- Patient assistance programs
- Membership discounts
- Financing options (CareCredit, medical loans)
- Provider-specific payment plans
These financial solutions make IV therapy accessible when facing high out-of-pocket costs or insurance denials.
How should you approach IV therapy and vitamin IV therapy options with The Drip IV Infusion?
The Drip IV Infusion provides comprehensive IV therapy services with transparent pricing and insurance support options. The clinic specializes in both medical IV treatments and wellness vitamin infusions, offering personalized consultations to determine the most appropriate therapy approach. Their medical team evaluates each client’s health goals and insurance coverage possibilities to create cost-effective treatment plans.
Can The Drip IV Infusion help with insurance verification or out-of-pocket options?
Yes. The Drip IV Infusion can help verify your insurance coverage and provide out-of-pocket payment options. Our billing specialists check your specific plan benefits, including deductibles, copayments, and prior authorization requirements for medically necessary IV treatments. For wellness vitamin IV therapy not covered by insurance, The Drip IV Infusion offers transparent self-pay pricing with package discounts for multiple sessions. We accept HSA and FSA payments for doctor-prescribed treatments with proper documentation. The clinic provides detailed receipts and can generate Letters of Medical Necessity when appropriate for reimbursement claims.
What are the key takeaways about IV therapy insurance coverage and vitamin IV therapy?
Understanding IV therapy insurance coverage helps you determine which treatments qualify as medically necessary and which fall under elective wellness care. Insurance companies cover IV treatments for documented medical conditions but exclude vitamin drips aimed at general wellness. Prior authorization remains a major factor, but most requests eventually get approved. By knowing your coverage requirements in advance, you can make informed decisions about your IV therapy options at The Drip IV Infusion.




