If you’re here looking up peripheral IV sites, you’re probably facing a medical procedure or helping someone who needs an IV. We get it – this stuff can feel scary. But you’ve come to the right place to learn exactly what these IV sites are and where doctors put them to take the best care of you.
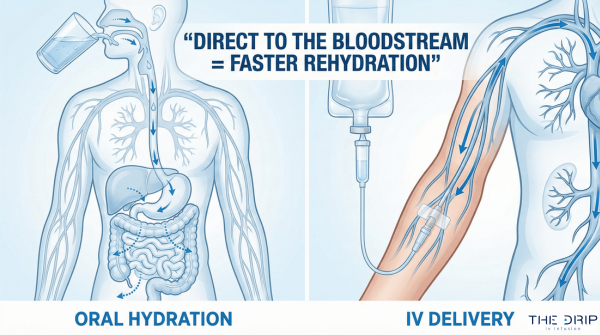
A peripheral IV site is just a spot on your body where doctors stick a tiny, bendy plastic tube into one of your veins. This lets them send fluids, medicines, or blood right into your bloodstream. Think of it like plugging a hose into your garden spigot. Unlike the big central lines that go deep near your heart, peripheral IVs use the veins in your arms, hands, or sometimes feet. They’re way less scary and the most common type – doctors use over 1 billion of them around the world each year.
TL;DR Summary:
- Peripheral IV sites are different from central lines because they use veins in your arms and hands instead of big vessels near your chest, making them less risky but good for shorter treatments
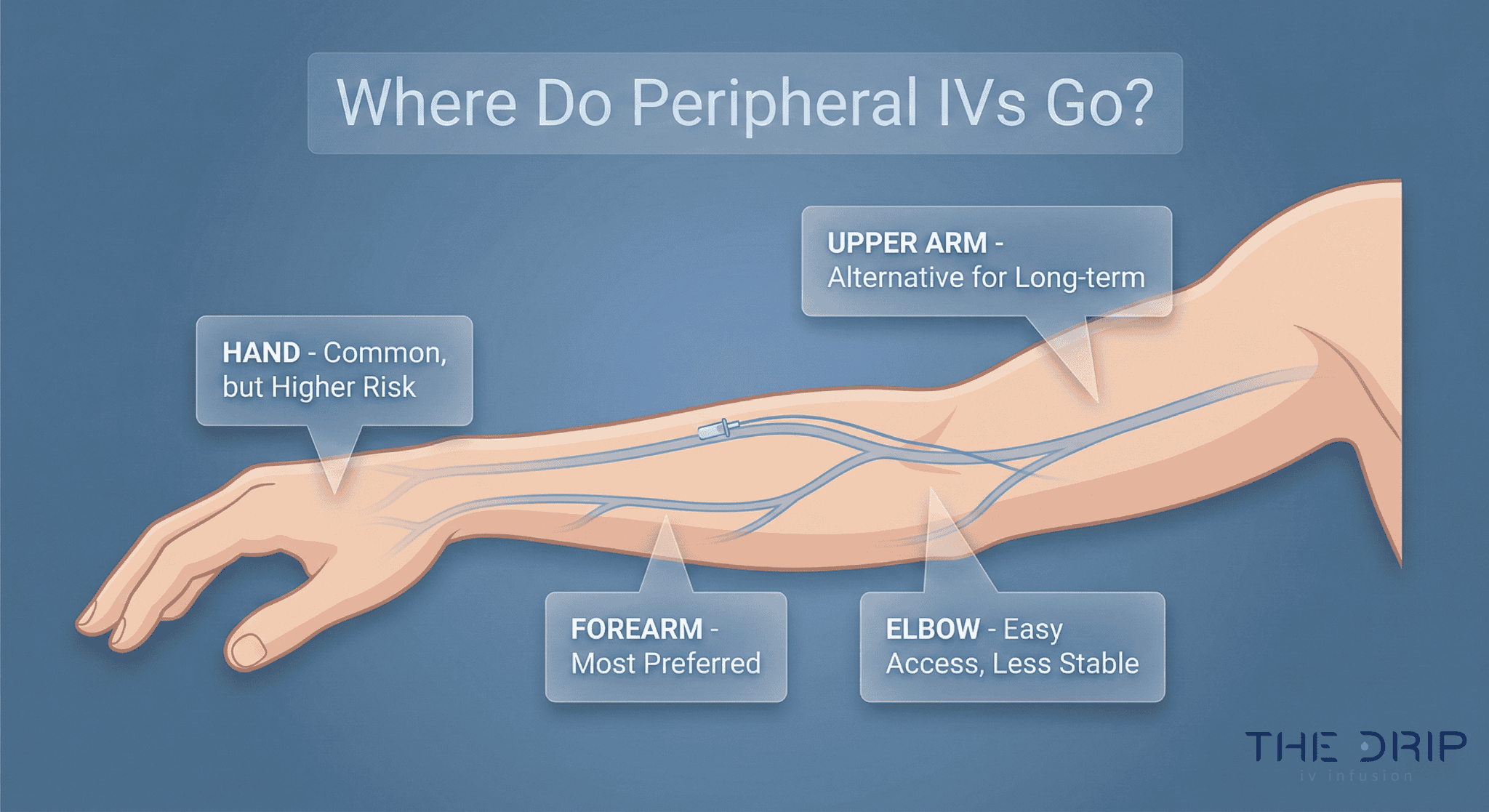
- Doctors group IV spots by where they are (hand, forearm, elbow area, upper arm, lower leg, scalp), with forearm spots being the best choice for most adults since they cause problems about 20% less often
- Good veins feel soft and bouncy, not hard or throbbing, and doctors like using your non-dominant arm so you can still use your main hand
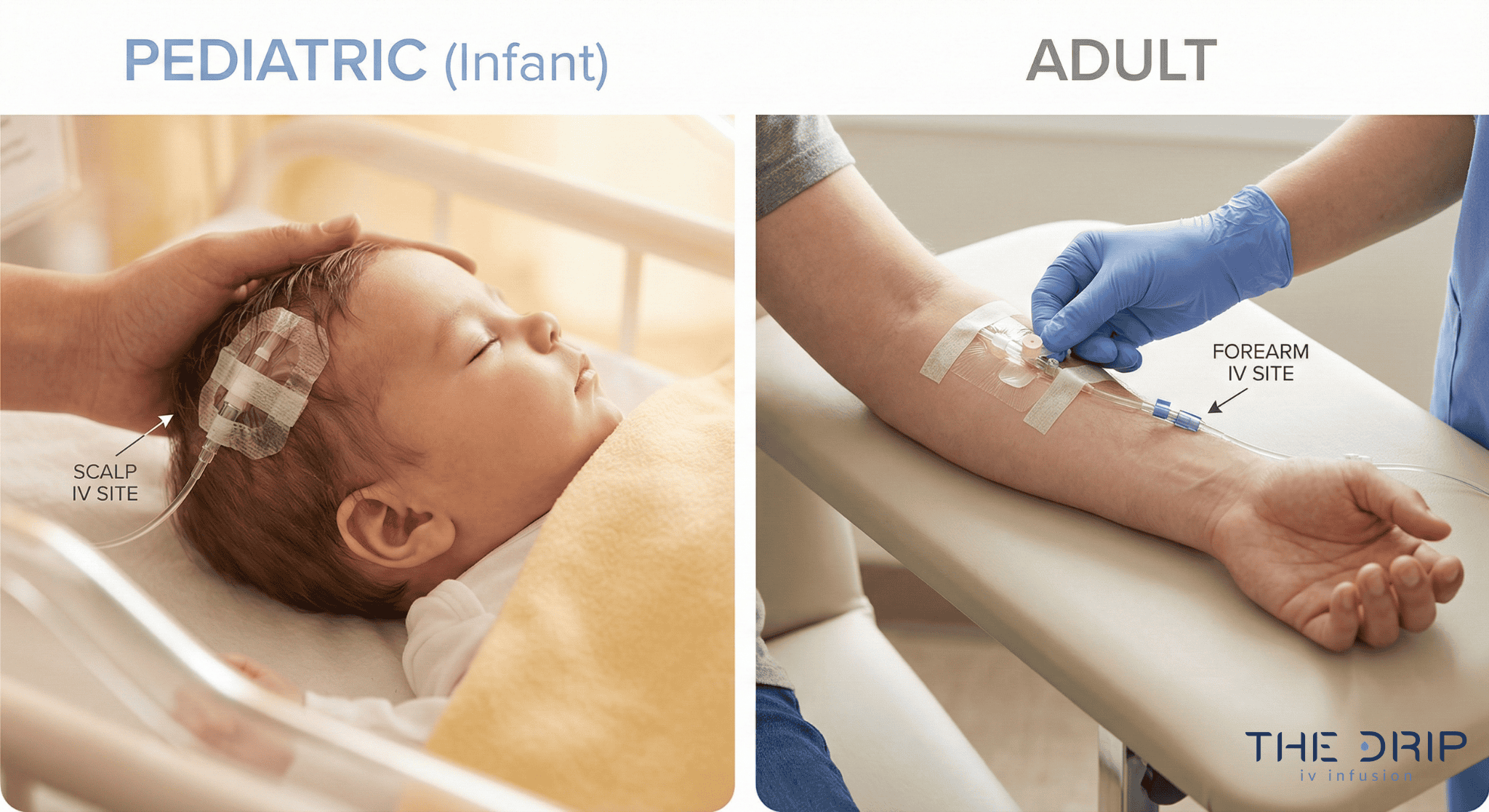
- Where they put your IV depends on your age, how good your veins are, how long you need treatment, and what’s wrong with you – older folks get about 7 out of 10 minor problems and 9 out of 10 major problems
- Common spots include hand veins on the back of your hand, arm veins in your forearm, and elbow veins (but only for emergencies)
- Forearm spots stay put better and don’t get messed up as easily as hand spots, though new research shows both work about the same overall
- Success rates are very different – doctors get it right 65-86% of the time in adults but only 53% in kids – using ultrasound helps them succeed over 90% of the time
- New technology that lets doctors see your veins better helps them get it right the first try and hurts less
- The Visual Infusion Phlebitis score helps doctors watch for problems on a scale from 0 to 5
- Professional IV services like The Drip IV Infusion use the best methods including vein-finding gadgets and different tricks to make veins bigger for easier placement
Quick Tip: When you get an IV, ask them to put it in your non-dominant forearm if they can. This spot usually feels the most comfortable, stays put better, and causes fewer problems while letting you keep using your main hand for everyday stuff.
As we dig into the details of where IVs go, you’ll understand why doctors pick certain spots, what happens when they put one in, and how the right spot makes you more comfortable and helps your treatment work better.
What defines a peripheral IV site and how is it different from other IV access points?
A peripheral IV site is a vein in your arms or legs where doctors put a single plastic tube to give you fluids, medicines, and blood. Over 1 billion of these plastic tubes help patients every year worldwide. About 8 out of 10 hospital patients get one.
Peripheral IVs are different from central lines because of where they go and how deep. Peripheral IVs go into veins in your arms, hands, or legs. Central lines go into big veins in your neck, chest, or groin and reach almost to your heart. Midline catheters are somewhere in between – they’re longer than regular IVs and go into your upper arm veins but stop before they get to your heart. PICCs work better for longer treatments but need special doctors to put them in.
These differences matter because peripheral IVs work great for short-term needs while central access helps with longer treatments.
How are peripheral IV sites categorized?
Peripheral IV sites are sorted by where they are on your body: hand, forearm, elbow area, upper arm, lower leg, and scalp veins for babies. Doctors like to use your non-dominant arm because it’s more comfortable for you, doesn’t get bumped around as much, and causes fewer problems.
What types of veins are typically chosen for peripheral IV placement?
Doctors look for straight veins that don’t branch off in your arms and legs. Good veins feel soft and squishy when they press on them, not hard or pulsing. Hard veins that feel like cords mean there’s a clot. Veins that pulse are actually arteries and doctors stay away from those.
Hand veins on the back of your hand are the farthest out, so doctors can try spots higher up your arm if the first one doesn’t work. Arm veins in your forearm are what most adults get. Elbow veins are saved for emergencies because bending your elbow can kink the tube.
What factors influence the choice of peripheral IV site?
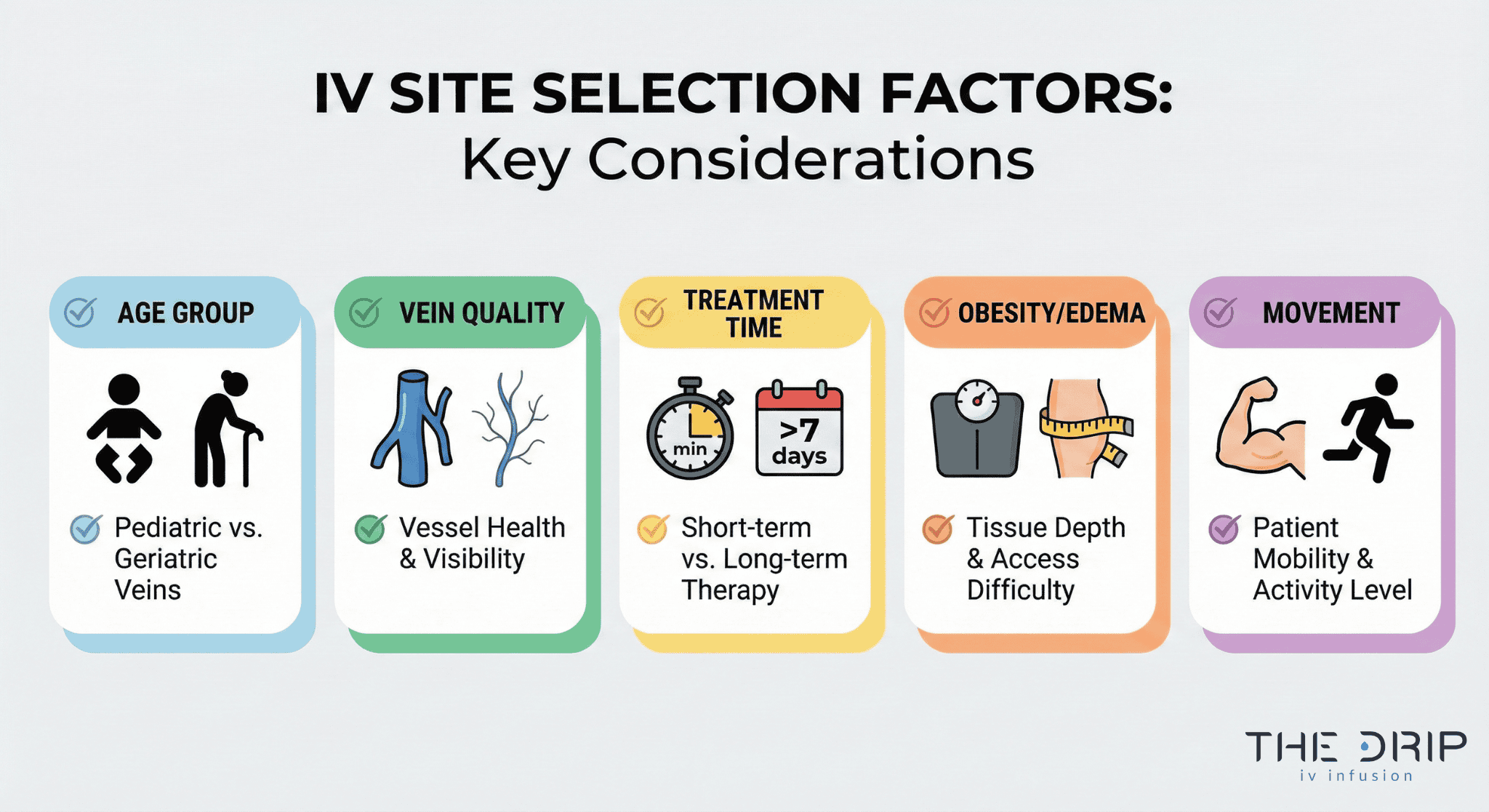
The factors that influence the choice of a peripheral IV site include patient age, vein quality, treatment duration, and medical history. Doctors consider several important factors when selecting a peripheral IV site. These factors affect success rates, patient comfort, and complication risks. Here are the main elements that guide the selection:
- Patient age and complication likelihood
- First-attempt success rates (varies by age group)
- Catheter size required for therapy
- Duration of therapy
- Vein accessibility challenges (e.g., obesity, drug use history)
- Phlebitis scoring from 0–5 to monitor inflammation
What are the main sites used for IV insertion on the body?
The main spots for IVs are your hand, forearm, elbow area, upper arm, lower leg, and scalp. Hand spots use veins on the back of your hand and are the farthest out, so doctors can try higher spots if needed. Forearm spots use bigger arm veins and are what most adults get because they cause fewer problems.
Elbow spots have big veins but doctors only use them in emergencies. Upper arm spots use the same veins that continue up your arm when other places won’t work. Lower leg spots include foot veins but doctors avoid these in adults unless they absolutely have to. Scalp veins work for babies and young kids when other spots can’t be used. These body areas are the foundation for where doctors decide to put IVs.
Why are certain anatomical sites preferred for IV insertion?
Certain anatomical sites are preferred because they offer safer access and better patient comfort. These preferences come from both evidence and clinical guidelines:
- Forearm veins have fewer complications
- Upper arm and hand veins have lower clot and swelling risk than leg veins
- The non-dominant arm minimizes disruption to daily activities
- CDC guidance prioritizes upper arm placement in adults
- Starting distally preserves more options if multiple attempts are needed
What are the advantages and disadvantages of the most common IV insertion sites?
Each spot has good and bad points with different problem rates. Forearm spots cause about 20% fewer problems like swelling, redness, and pain compared to hand spots. Hand spots cause over half of both minor and major IV problems even though doctors use them a lot. Elbow spots can get kinked when you bend your arm, which stops the flow and causes problems.
Leg spots have higher chances of infection and blood clots in adults, so doctors don’t like using them. A 2023 study found that overall, forearm and hand spots have about the same problem rates, which means how well the doctor does it and takes care of it matters just as much as where it goes.
What complications are associated with different IV insertion locations?
Complication risks and dwell-time performance vary by IV location and device type. The table shows the major measurable values:
| Element | Measurement | Value |
| Swelling rate | Forearm vs Hand | Similar |
| Infiltration rate | Forearm vs Hand | Similar |
| Problem distribution | Hand/Wrist | >50% of issues |
| Average dwell time | Standard IVs | 73 hours |
| Dwell time | Closed-system | 137 hours |
| Dwell time | Regular system | 96 hours |
What should be considered when choosing IV sites on the forearm?
Picking forearm IV spots means looking at your blood vessels, your specific situation, and how to put it in. The two main arm veins serve as the primary vessels for forearm IVs. Medical guidelines say the forearm is the best spot for most adults. A 2023 study found problems happen about 20% less often in forearm IVs compared to hand placement. Medical standards limit doctors to two attempts per person to minimize trauma.
Doctors check vein quality by feeling and looking before picking spots. Good forearm veins feel soft, bouncy, and stretchy rather than hard or like cords. Your non-dominant arm works better for comfort and less chance of it getting knocked out. These body and practical considerations guide doctors toward the best forearm IV placement.
How do forearm veins compare to hand veins for IV insertion?
Forearm and hand veins differ in complication profiles and practical performance. The table below summarizes the most important measurable differences between these two IV sites:
| Site | Complication Rate | Key Study Findings | Stability During Movement |
| Forearm | ~20% fewer issues | 2023 study: no significant difference overall | More stable |
| Hand | >50% of minor & major issues | Same 2023 study: comparable outcomes | Less stable |
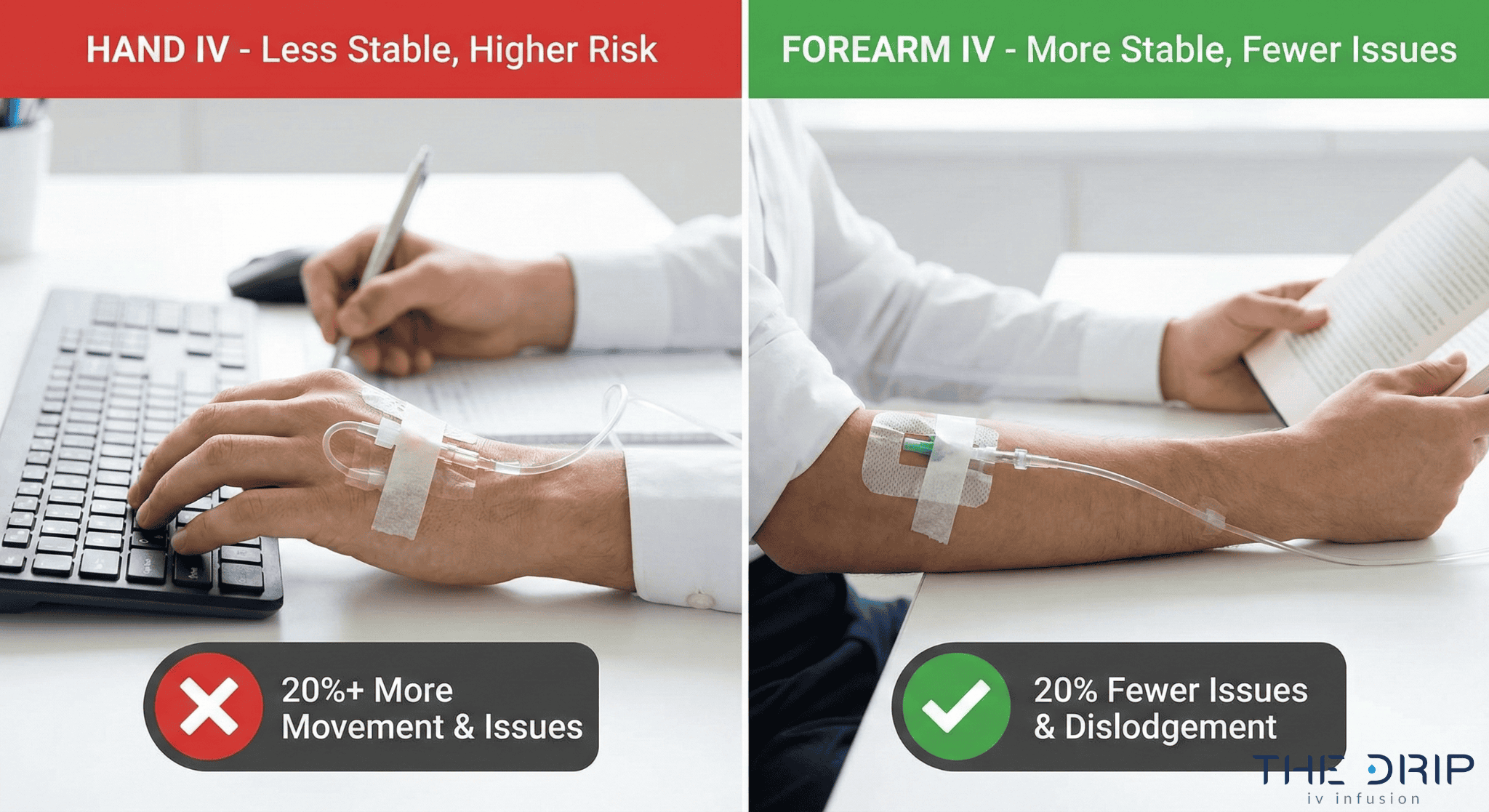
What are the benefits and risks of forearm IV sites?
Forearm IV spots are easy to secure and less likely to get knocked out when you move around. Forearm placement lets you keep using your hand for daily activities like eating, writing, and using your phone. A 2023 analysis found no real difference in swelling rates between forearm and hand spots. The same study showed no real difference in fluid leaking rates between forearm and hand spots either.
Risk factors stay minimal when doctors use proper technique. Your specific situation like vein quality, skin condition, and how much you move around influences where they put it. These balanced benefits and risks make forearm spots optimal choices for most adult patients who need IVs.
What techniques help ensure successful IV placement in the forearm?
Several techniques help doctors achieve successful forearm IV placement. These methods improve vein visibility and accessibility, increasing first-attempt success:
- Applying a tourniquet
- Palpating for soft, bouncy veins
- Positioning the arm so gravity fills the veins
- Warming the site
- Gently tapping to stimulate dilation
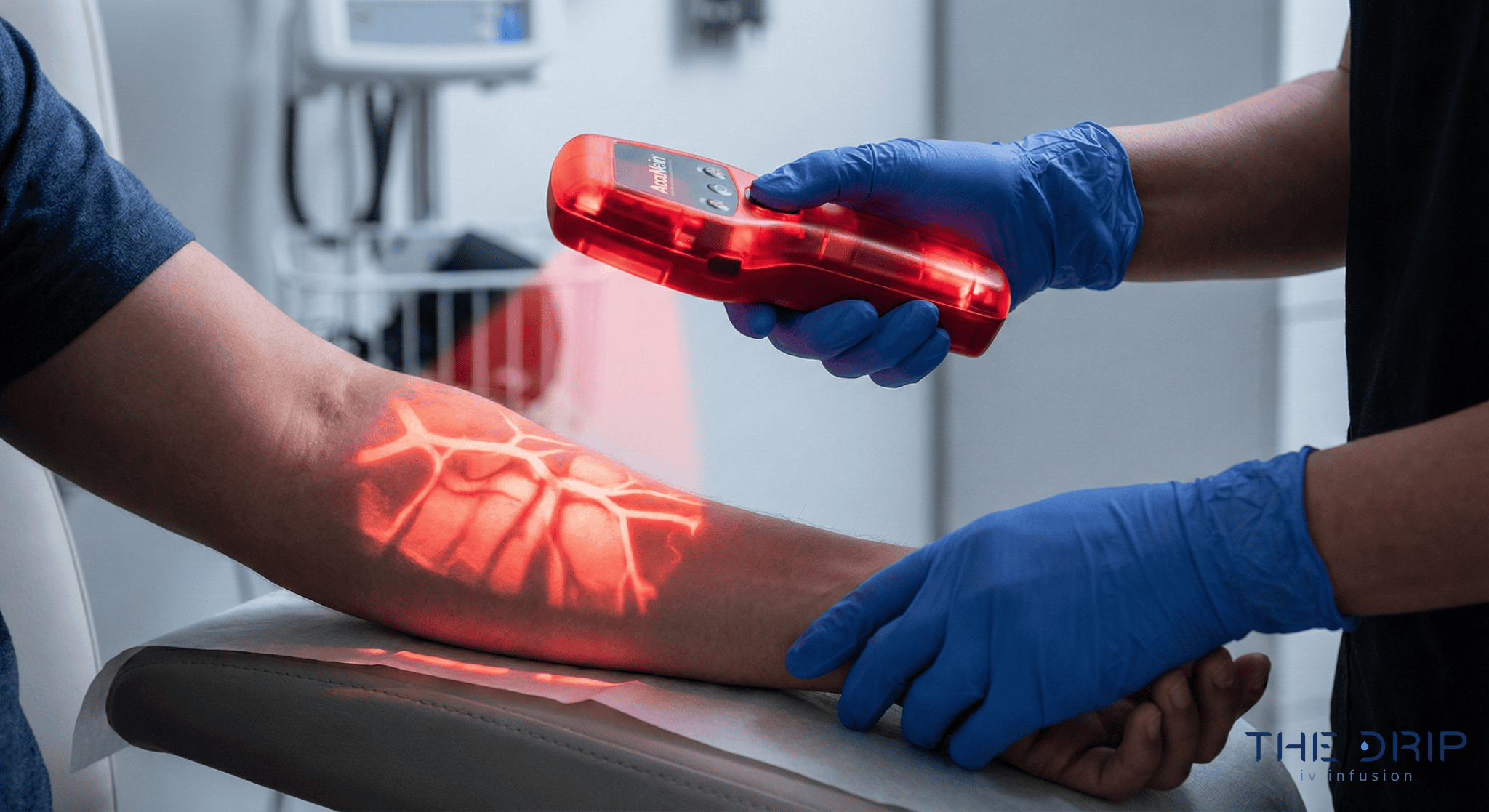
- Using ultrasound or vein-finding technology as needed
Near-infrared vein finders like AccuVein help doctors succeed on the first try while reducing pain and stress. Vein visualization devices project real-time maps of your blood vessels onto your skin so they can identify the best veins. These technologies work alongside traditional assessment methods to optimize forearm IV placement. The combination of hands-on techniques and advanced visualization tools enhances forearm IV placement outcomes across all kinds of patients.
How should you approach peripheral IV site selection and care with The Drip IV Infusion?
The Drip IV Infusion picks IV spots using evidence-based ways to check your veins. The service focuses on your non-dominant arm for comfort and less chance of it getting knocked out. Trained professionals check vein quality by feeling for soft, bouncy, and stretchy vessels that show healthy blood flow. The Drip IV Infusion uses advanced vein finder technology to project real-time maps of your blood vessels onto your skin surface. These near-infrared devices help them succeed on the first attempt while reducing discomfort. The upcoming sections detail their specific selection criteria and management techniques.
Can The Drip IV Infusion help with choosing and managing peripheral IV sites?
Yes. The Drip IV Infusion can help with choosing and managing peripheral IV sites by following Infusion Nurses Society standards for vein assessment. Their practitioners pick non-dominant upper arm sites to keep you mobile during infusion sessions. The service uses multiple vein enhancement techniques including tourniquet application, gravity positioning, local warming, and gentle tapping to make veins more visible.
Vein finder technology provides visual confirmation of suitable vessels before they try to insert anything. The Drip IV Infusion limits insertion attempts to two per practitioner, following INS guidelines. Their systematic approach combines hands-on assessment with technological visualization for optimal site selection.
What are the key takeaways about peripheral IV sites, IV insertion locations, and forearm IV sites we covered?
The key takeaways about peripheral IV sites include their status as the most frequently performed invasive procedure with over 1 billion used annually worldwide. Forearm spots cause about 20% fewer complications compared to hand placement locations. First-attempt success rates range from 65-86% in adults versus 53% in kids.
The Visual Infusion Phlebitis score provides standardized assessment from 0-5 for monitoring insertion sites. Ultrasound guidance achieves success rates exceeding 90% for difficult access cases. Average time in place reaches 73 hours for standard IVs, extending to 137 hours with closed-system devices. CDC and medical standards recommend upper arm placement using the smallest appropriate size for the prescribed therapy.