The history of IV therapy is the 300-year progression from early animal experiments in 1656 to the modern, life-saving medical treatment used worldwide today. If you’re curious about how IV therapy went from wild animal experiments to something that saves your life, you’re in the right spot. Maybe you’re doing research, thinking about getting IV therapy, or just love medical stories – either way, we’ll walk you through an amazing 300-year journey that turned crazy experiments into the healthcare basics you see today.
The history of IV therapy is basically the story of how doctors figured out how to put fluids directly into your veins without killing you. Back in 1656, it was super dangerous stuff, but now it saves millions of people every year with less than 1% of folks dying from things that used to kill more than half.
TL;DR Summary: IV therapy started when Sir Christopher Wren stuck goose quills and pig bladders into animals in 1656, got a major boost when Dr. Thomas Latta saved cholera patients in 1832 with a 57% survival rate, got way better when Baxter made flexible plastic IV bags in 1970, and went from scary experiments to everyday medical stuff that dropped cholera deaths from over 50% to less than 1% while saving millions through better fluid management.
The trip from basic injections to fancy medical systems shows you how science, desperate need, and smart engineering work together. Early doctors risked everything testing sketchy methods during deadly outbreaks. Their guts laid the groundwork for stuff we totally take for granted now – like the Rochester needle that made long-term IVs comfortable or those closed plastic bags that stopped contamination. Getting this history helps you appreciate why modern IV therapy services like The Drip IV Infusion can safely give you treatments that once seemed like magic.
How Did IV Therapy Originate and Evolve Over Time?
IV therapy started in 1656 when Sir Christopher Wren did the first documented IV injections at Oxford University. William Harvey figured out how blood circulation worked in 1628, which basically made IV therapy possible in the first place. The whole thing changed from scary animal experiments into life-saving standard medicine over three centuries. Early methods went from crude tools to sophisticated closed systems, dropping death rates from 40-70% to less than 1% for stuff like cholera.
What Were the Earliest Methods of Intravenous Therapy?
The earliest IV methods had Sir Christopher Wren using a goose quill stuck to a pig’s bladder to inject wine, ale, and opium into dogs’ veins back in 1656 at Oxford. William Harvey’s 1628 discovery of how blood moves around your body set up the science for IV development. That story you might’ve heard about Pope Innocent VIII getting blood transfusions in 1492? Total made-up nonsense from anti-Semitic propaganda. These basic experiments showed that stuff injected straight into your bloodstream affected your whole body, setting up the groundwork for medical uses.

How Have IV Therapy Practices Changed Throughout History?
Mortality outcomes from cholera treatment show how IV therapy revolutionized patient survival. The comparison highlights the sharp improvement achieved through saline administration and sterile practice.
| Time Period | Treatment Method | Outcome |
| Pre-1832 | Bloodletting, purging | 40–70% mortality |
| 1832 (Latta) | IV saline | 57% survival |
| Modern era | IV therapy + ORT | <1% mortality |
IV therapy practices changed from harmful bloodletting to smart fluid replacement over two centuries. Before 1832, cholera treatments relied on bleeding people and purging with death rates of 40-70%. Dr. Thomas Latta got a 57% survival rate in 1832 cholera patients using IV saline, treating 14 really sick patients with 8 survivors. Modern cholera treatment with IV therapy gets less than 1% death rate compared to 30-84% in the late 1800s and early 1900s. A 2018 WHO report showed kids’ diarrhea deaths dropped from over 5 million yearly pre-1980s to under 500,000 through better IV and oral rehydration access.

What Major Medical Discoveries Influenced IV Therapy’s Development?
The big medical discoveries that shaped IV therapy were figuring out what’s in your body fluids, sterile techniques, and understanding electrolyte balance. Dr. W.B. O’Shaughnessy’s 1831-1832 chemical analysis found severe water and salt shortage in cholera patients’ blood, proving why saline replacement made sense. Sterile techniques in the late 1800s cut down sepsis complications from IV administration. Understanding fluid and electrolyte balance in the mid-1900s made consistent life-saving outcomes possible. These discoveries changed IV therapy from experimental treatment to standard medical practice that saves millions of lives every year.
When Were IV Bags Invented and Why Are They Important?
IV bags got invented in 1970 when Baxter Laboratories introduced VIAFLEX®, the first flexible plastic IV container made from poly(vinyl chloride) stuff. This innovation replaced glass bottles that had been running medical practice for decades, totally changing how healthcare providers deliver IV fluids worldwide.
What Problems Did IV Bags Solve in Medical Practice?
Glass bottles introduced several major obstacles for early IV therapy. These issues affected safety, storage, and usability in clinical settings. The main problems included:
- Heavy weight that burdened staff
- Frequent breakage during transport
- Requirement for air-inlet needles that increased contamination
- Bulky storage needs that limited inventory
- Open-system design that raised infection risks
Storage and moving challenges limited IV therapy access. Glass containers broke all the time during shipping, wasting valuable medical supplies. Hospital staff struggled with the weight of glass bottles, especially when moving multiple units around. The rigid shape of bottles also ate up way too much storage space in medical facilities.
The contamination pathway from air-inlet needles created serious infection risks. Each bottle needed a separate venting system that exposed sterile fluids to environmental nasties. This open-system design contributed to higher rates of bloodstream infections and sepsis complications.

How Did the Invention of IV Bags Transform IV Therapy?
The introduction of IV bags brought several transformative improvements to medical practice. These enhancements made IV therapy safer, more portable, and easier to manage. Key advantages included:
- A closed system that eliminated air contamination
- Flexible plastic that collapsed naturally as fluid infused
- Lightweight design improving storage efficiency
- Break-resistant construction enabling safe transport
- Longer drug stability from multilayer plastic films
Lightweight and tough plastic bags made storage and administration way easier. Medical facilities could store more IV fluids in less space, cutting inventory costs. The unbreakable nature of plastic bags enabled safer transportation to remote locations and disaster zones.
W.D. Johnston got patents for related film laminates in the 1980s, specifically U.S. Patents 4,686,125 and 4,692,361. These patents advanced multilayer plastic technology that improved drug stability and made stuff last longer. The closed-system design significantly cut infection rates by getting rid of the air-inlet contamination pathway present in glass bottles.
This revolutionary packaging system made IV therapy more accessible and safer, setting up the foundation for modern intravenous treatment protocols used globally today.
Who Invented the IV and What Was Their Contribution?
The invention of IV therapy came together through contributions from multiple pioneering doctors and scientists across centuries. Sir Christopher Wren did the first documented IV injections in 1656 at Oxford University, showing that stuff injected directly into veins could affect your whole body. Dr. Thomas Latta became the first doctor to successfully treat human patients with IV saline in 1832, while Dr. David J. Massa developed the first modern over-the-needle IV catheter at Mayo Clinic in 1950. These three key guys established the foundation, clinical application, and modern safety standards that define IV therapy today.
What Key Figures Shaped the Invention of IV Therapy?
Sir Christopher Wren pioneered IV therapy in 1656 by doing the first documented IV injections on dogs at Oxford University. Wren crafted basic IV equipment using goose quills attached to pig bladders, successfully showing that substances introduced directly into your bloodstream produced immediate effects throughout your body. His experiments proved IV drug delivery worked centuries before medical acceptance.
Dr. Thomas Latta revolutionized human medicine in 1832 as the first doctor to successfully treat patients with IV saline during Scotland’s cholera epidemic. Latta modified enema syringes and crafted silver needles to deliver saline solutions directly into patients’ veins. His treatment of 14 severely ill cholera patients in Leith achieved an unprecedented 57% survival rate when standard treatments yielded 40-70% mortality.
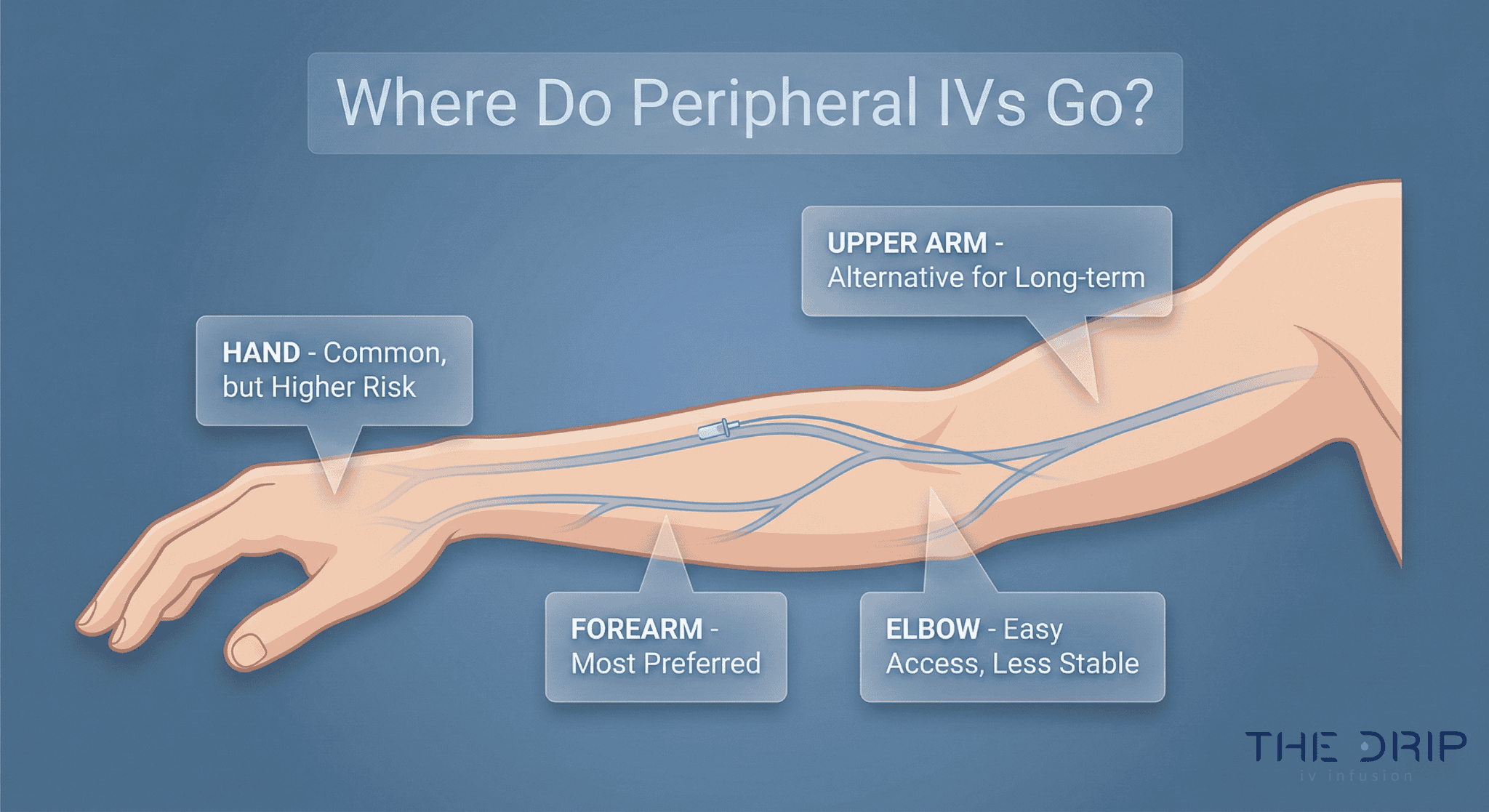
Dr. David J. Massa transformed IV safety in 1950 by developing the Rochester needle, the first over-the-needle catheter, at Mayo Clinic. Massa’s innovation allowed the plastic catheter to stay in your vein after needle withdrawal, reducing vein damage and infiltration complications. Despite the device’s revolutionary impact on patient care, Massa never patented his invention, allowing widespread adoption that benefits millions of patients every year.
How Did Early Inventors Test and Popularize IV Use?
Early inventors tested IV therapy through animal experiments and emergency medical situations that demanded innovative approaches. Wren conducted extensive experiments on dogs, injecting wine that made them “extremely drunk” and testing the effects of opium and scammony to understand how IV delivery affected drug action. These experiments established fundamental principles of IV pharmacology that guide modern practice.
Dr. Latta’s clinical application emerged during the 1831-1832 cholera epidemic in Leith, Scotland, where conventional treatments failed catastrophically. Latta treated 14 patients in critical condition with IV saline, achieving survival in eight cases despite their severe dehydration and near-death status. His detailed case reports published in The Lancet provided the first clinical evidence supporting IV fluid resuscitation.
IV saline practice largely vanished for over 50 years following Latta’s death in 1833 due to medical establishment skepticism and lack of sterile technique understanding. The medical community rejected IV therapy despite Latta’s documented success, preferring traditional but ineffective treatments like bloodletting and purging. This resistance delayed IV therapy adoption until germ theory and sterile techniques emerged in the late 1800s, finally validating the inventors’ pioneering work and establishing IV therapy as standard medical practice.
What Are the Major Milestones in the Advancements of IV Therapy?
The major milestones in IV therapy advancements include the 1950 development of plastic catheters, the 1970 introduction of closed-system plastic bags, and the expansion of IV therapy into a $50 billion global market by 2024. These innovations transformed IV therapy from a hospital-only treatment to something you can get almost anywhere. The following sections explore how IV therapy expanded beyond clinical settings and which tech breakthroughs made treatment safer.
How Did IV Therapy Expand Beyond Hospitals?
IV therapy expanded beyond hospitals through commercialization of wellness treatments and adaptation of its principles for global health initiatives. The global IV therapy and venous access devices market reached over $50 billion valuation by 2024. FDA raised alarms in 2024 about wellness IV treatments at unregulated med spas, highlighting rapid growth outside traditional healthcare settings. Development of Oral Rehydration Therapy (ORT) based on IV therapy principles saved millions of lives globally by making treatment accessible in resource-limited areas. This expansion shows how IV therapy evolved from emergency medicine to preventive wellness care.

What Technological Innovations Enhanced IV Safety and Effectiveness?
Modern IV therapy safety stems from several major technological and regulatory advances. These improvements addressed catheter stability, contamination, and quality control. Notable innovations include:
- Plastic over-the-needle catheters introduced in 1950
- Closed-system IV bags developed in 1970
- FDA regulation of IV fluids and devices
- Infusion Nurses Society (INS) evidence-based standards
These advances reduced complications from over 30% in early treatments to less than 1% today.
How Does Modern IV Therapy Differ From Historical Practices?
Modern IV therapy differs from historical practices through sterile closed-system technology, standardized formulations, and evidence-based protocols that reduced death rates from 30-70% to under 1%. The transformation from experimental glass bottles to regulated plastic bags revolutionized patient safety and treatment accessibility.
What Are Today’s Common Uses for IV Therapy?
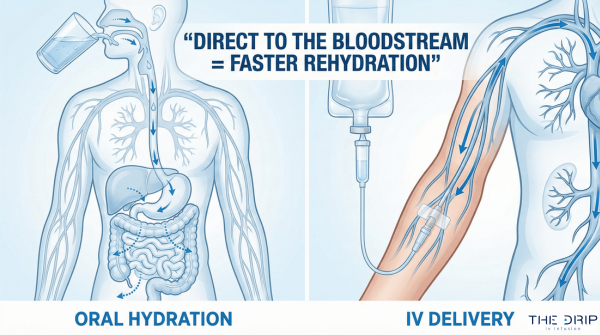
Today’s common uses for IV therapy include rehydration, antibiotic delivery, chemotherapy administration, and parenteral nutrition support. IV therapy serves as cornerstone treatment across emergency departments, surgical units, and outpatient clinics nationwide.
Modern applications show remarkable success rates. In 1971, refugee camps achieved 3.6% cholera mortality using modern IV and oral rehydration therapy versus 30% mortality in untreated camps. Healthcare facilities address periodic fluid shortages through strategic IV therapy protocols.
Common IV treatments include:
• Crystalloid solutions for dehydration and electrolyte imbalance
• Antibiotic infusions for severe infections
• Chemotherapy drugs requiring precise dosing
• Total parenteral nutrition for patients unable to eat
This versatility makes IV therapy essential for treating conditions ranging from simple dehydration to complex medical emergencies.
How Has Patient Care Improved With Current IV Methods?
Patient outcomes improved through multiple advancements in safety, equipment, and protocol design. These updates eliminated contamination pathways and reduced complications. The most important improvements include:
- Sterile disposable equipment
- Flexible plastic catheters for long-term use
- Standardized electrolyte formulations
- Professional practice standards from the INS
These advances got rid of the sepsis complications that plagued early IV attempts when practitioners reused needles and lacked sterilization protocols.
Flexible plastic catheters allow long-term venous access without repeated needle sticks that damaged veins in historical practice. Modern catheters stay in place for days, reducing your discomfort and infection risk. Standardized fluid and electrolyte formulations ensure consistent treatment outcomes across facilities.
Professional organizations transformed IV therapy safety standards. The Infusion Nurses Society guides clinical practice through evidence-based protocols and enhances clinician competency via specialized certification programs. These standards include:
• Aseptic technique requirements
• Catheter selection guidelines
• Complication prevention protocols
• Documentation standards for legal compliance
Modern IV therapy’s systematic approach contrasts sharply with the experimental methods of the 1800s, when doctors mixed their own solutions without understanding electrolyte balance or contamination risks.
How Can Learning the History of IV Therapy Benefit Patients Today?
Learning the history of IV therapy benefits you today by showing how centuries of medical innovation created the safe, effective treatments now available. The evolution from Christopher Wren’s 1656 goose quill experiments to modern sterile systems shows you why current protocols exist. Understanding IV therapy’s development helps you appreciate safety standards that prevent the sepsis complications that killed early recipients. Historical knowledge shows you why regulated facilities matter—unregulated IV administration caused numerous deaths before sterile techniques emerged in the late 1800s.
You gain confidence knowing your treatments build on proven scientific foundations. The transformation of cholera mortality from 70% to under 1% through IV saline validates the therapy’s effectiveness. Modern IV therapy incorporates lessons from past failures, such as contamination from open glass bottle systems, which plastic bags eliminated in 1970. This historical perspective empowers you to make informed decisions about your care options.
How Does The Drip IV Infusion Incorporate Historic Innovations Into Its Services?
The Drip IV Infusion incorporates historic innovations into its services through sterile closed-system technology descended from Baxter’s 1970 VIAFLEX® containers. The facility uses flexible plastic bags that got rid of the contamination risks of glass bottles requiring air-inlet needles. Modern over-the-needle catheters, evolved from Dr. David Massa’s 1950 Rochester needle design, allow comfortable venous access without repeated punctures.
The Drip IV Infusion applies electrolyte formulations refined from Dr. W.B. O’Shaughnessy’s 1831 discovery of salt and water deficiency in dehydrated patients. Professional standards developed by the Infusion Nurses Society guide clinical practices at the facility. Safety protocols stem from late 1800s sterile technique developments that reduced sepsis from IV administration. These historic foundations ensure you receive treatments proven through three centuries of medical advancement.
What Are the Most Important Insights About the History of IV Therapy?
These milestones show how the history of IV therapy reveals a steady progression of scientific discovery, engineering innovation, and clinical practice that now saves millions of lives every year. IV therapy’s evolution shows how theoretical concepts transformed into practical tools through persistent innovation. Cholera treatment success proved IV therapy’s potential by reducing mortality from over 50% to less than 1% through saline administration.
Baxter Laboratories’ founding in 1931 as the first commercial manufacturer of prepared IV solutions pioneered modern IV delivery systems. The company’s 1970 introduction of flexible plastic containers revolutionized safety by eliminating contamination pathways. Engineering advances like the Rochester needle enabled long-term venous access without vein damage. These milestones show you how each innovation built upon previous discoveries to create today’s sophisticated IV therapy systems that save millions of lives every year.