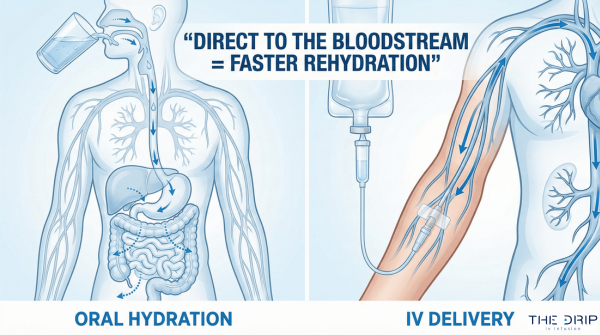
If you’re reading this, you’re probably getting ready for a medical procedure, worried about getting an IV, or just want to understand what doctors and nurses think about when they pick the right needle for you. Maybe you’re nervous about how much the needle will hurt, curious about how fast different treatments flow, or need to know the technical stuff for work. We’ve put together everything you need to know about IV needle sizes so you feel ready and informed.
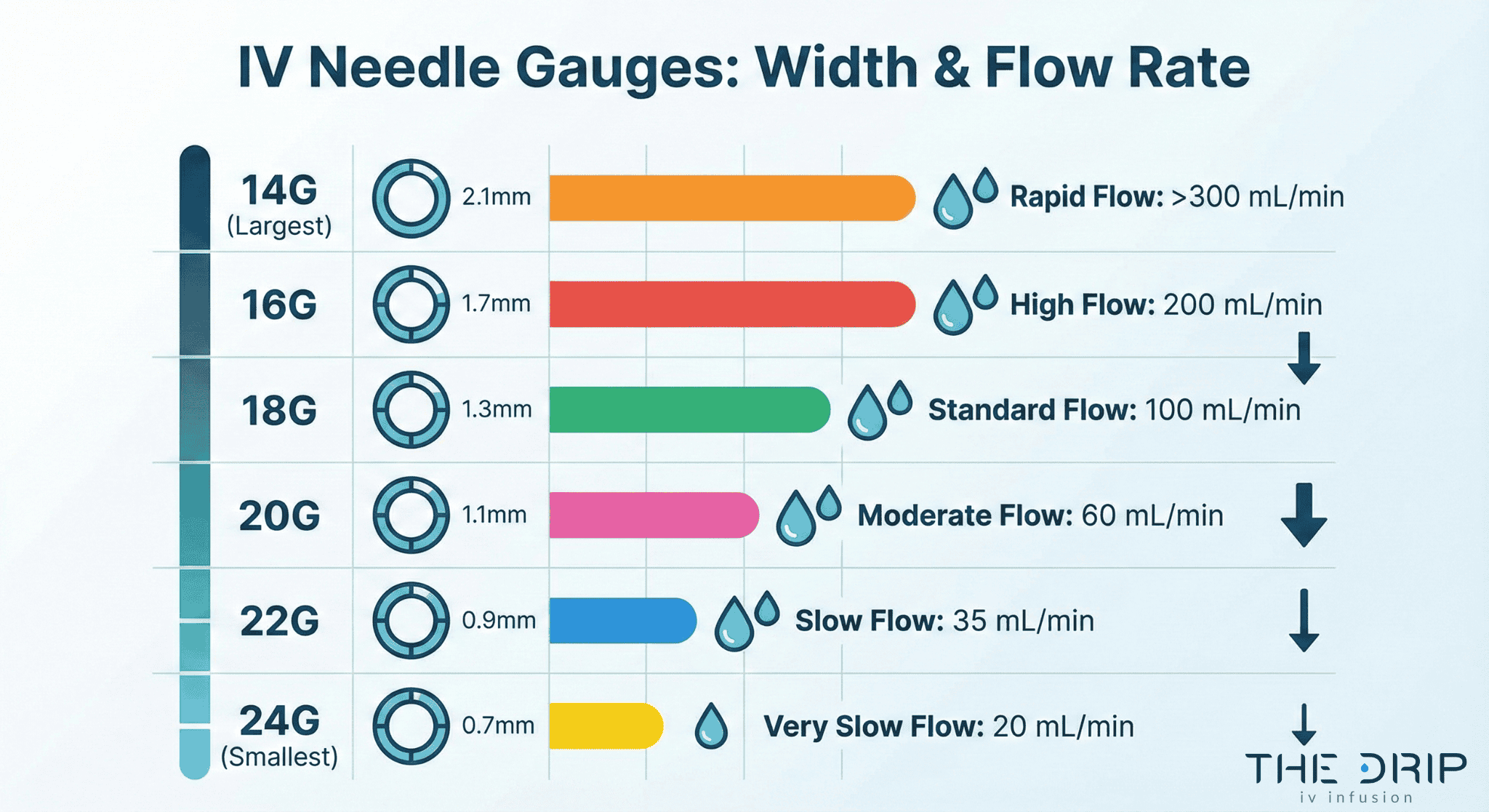
IV needle sizes are like a measuring system that sorts intravenous catheters by how wide they are using gauge numbers. The sizes usually go from 14G (biggest) to 24G (smallest), where smaller numbers mean bigger needle widths and faster flow rates—something healthcare providers think about when matching needle size to your specific treatment and what your body needs.
TL;DR Summary:
Understanding IV needle sizes helps make your medical care safer and more comfortable. Here’s what we cover:
- Gauge measurements and what they mean: IV needles range from 14G-24G, with smaller numbers meaning bigger widths—14G delivers 240 mL/min for trauma cases while 24G delivers 20 mL/min for delicate veins
- Why picking the right size matters: The right needle size affects how comfortable you are, your safety, and whether your treatment works—with 35-50% of IV catheters failing because of problems, choosing the right size cuts down risks of infiltration, phlebitis, and the catheter coming out
- Common sizes by where you get care: Adults usually get 20G-22G for routine care, 18G-20G for blood transfusions, while kids use 22G-24G sizes to be gentler on their veins
- How providers decide: Healthcare teams look at your age, vein condition, medication type, and how urgent your treatment is using tools like the A-DIVA scale to predict difficult access and pick the right sizes
- How different devices compare: Peripheral IVs use gauge sizing while central lines use French measurements, with different materials and flow rates affecting how they work in practice
- Best ways to insert them: Following 2024 INS Standards means picking the smallest size that works, using ultrasound guidance for tough access, and making sure to throw them away properly in FDA-approved sharps containers
- Professional guidance: Expert agreement from AVA, INS, and AACN emphasizes reducing complications through proper size selection, with The Drip IV Infusion following these evidence-based standards for the best patient care
Quick Tip: When talking about IV placement with your healthcare provider, ask about their needle size recommendation and why they picked it—understanding why a specific gauge is chosen for your treatment can help calm your nerves and make sure you’re getting the right care based on your individual vein condition and treatment needs.
What Are the Different Sizes of IV Needles and How Are They Measured?
The different sizes of IV needles are measured using gauge numbers, French sizing, and how long they are. IV catheter gauges range from 14G to 24G, with 14G having an outer width of 2.1mm and 24G having an outer width of 0.7mm (Lippincott NursingCenter, 2025). The smaller the gauge number, the bigger the catheter width, which lets more fluid flow through faster. Understanding these measurements helps healthcare providers pick the right needles for specific medical needs.
How are IV needle gauges sorted?
IV needle gauges are sorted by width using a backwards numbering system. Standard peripheral IV catheters use gauge sizing from 14G to 24G (Lippincott NursingCenter, 2025). Rapid Infusion Catheters (RICs) measure 7-Fr (roughly 13.3Ga) and 8.5-Fr (roughly 11.8Ga) with lengths of 5-6.4cm (EMRA Critical Care Device Series, 2025). Central Venous Catheters usually use French sizing, with 8 French introducers measuring 2.8mm across (Lippincott NursingCenter, 2025). This sorting system lets doctors and nurses quickly figure out what a catheter can do based on standard measurements.
What do the different gauge numbers mean?
The different gauge numbers tell you specific flow rates and what they’re used for in medicine.
| Gauge Size | Outer/Inner Width | Typical Flow Rate | Common Use |
| 14G | ~2.1 mm | ~240 mL/min | Trauma / rapid resuscitation |
| 16G | 1.32–1.39 mm | Very high | Emergency rapid infusion |
| 20G | ~0.9 mm | ~60 mL/min | Routine fluids / meds |
| 22G | 0.61–0.69 mm | Moderate | Elderly / small veins |
| 24G | 0.7 mm outer | ~20 mL/min | Pediatrics / fragile veins |
How does needle length factor into size selection?
Needle length directly affects flow rates and medical uses through Poiseuille’s law. Standard peripheral IV catheter lengths range from 0.75 inches for 24G to 1.75 inches for 14G catheters (BD Product Specifications, 2025). RICs measure 5-6.4cm long, shorter than central introducers, which makes flow rates faster (EMRA, 2025).
PICC lines show slower flow rates of 20-65 mL/min because of their extended length and small width (Lippincott NursingCenter, 2025). Neonatal long peripheral catheters (n-LPCs) are specifically designed for longer stays with better stability (van Rens et al., 2025). These length differences let healthcare providers match catheter choice to your body’s anatomy and how long your treatment needs to last.
Why Does Choosing the Correct IV Needle Size Matter?
Choosing the correct IV needle size matters because it directly affects how comfortable you are, your safety, and whether your treatment works. The Association for Vascular Access recommends picking the smallest size that meets your medical needs to reduce complications (AVA Standards of Care, 2024).
A 2021 study at Queensland hospitals found that 22/24 gauge catheters showed 27% increased risk of all-cause failure compared to bigger gauges (Marsh et al., 2021). The following sections explore how needle size affects your comfort, fluid flow rates, and potential problems.
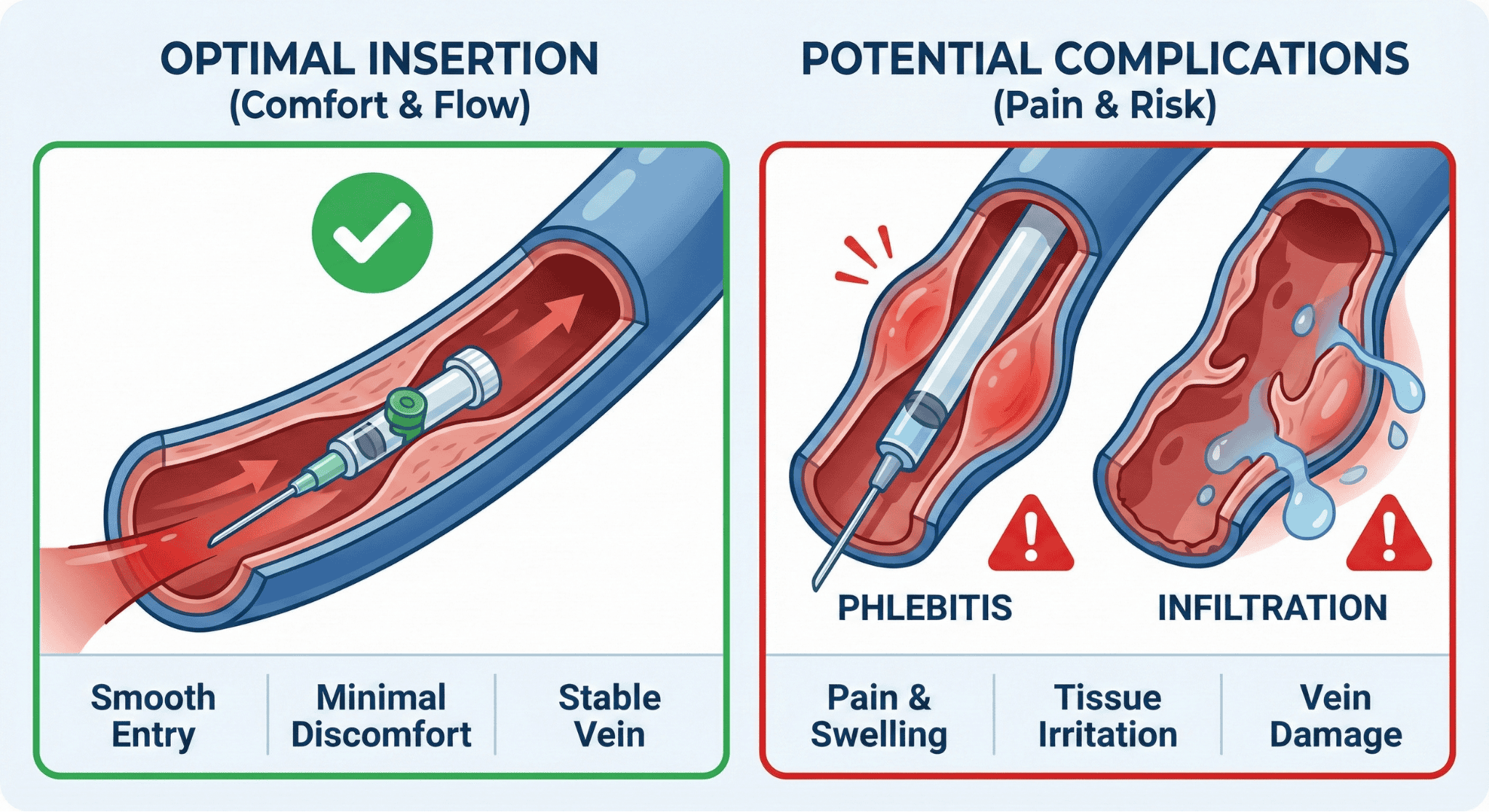
How does needle size affect patient comfort and safety?
Needle size affects your comfort and safety through insertion trauma, vein damage, and complication rates. Smaller gauge needles cause less pain when they go in but might increase failure rates. A 2021 randomized controlled trial on peripheral IV catheters found female patients experience higher complication rates with phlebitis (HR 1.98) and infiltration/occlusion (HR 1.45) compared to males (Marsh et al., 2021). Vascular access teams reduce the risk of catheters coming out by 47% (HR 0.53) compared to other providers (Marsh et al., 2021). The smallest size that works minimizes vein trauma while keeping your treatment effective.
What impact does needle size have on fluid flow rates?
Needle size has a big impact on fluid flow rates through width-dependent flow physics. Think of it like water flowing through different sized straws—bigger straws let more water through faster. Larger bore catheters deliver faster flow rates following Poiseuille’s law.
This comparison highlights flow ranges across device categories:
| Device Type | Flow Capacity | Notes |
| Standard IV Set | Up to 12,000 mL/hr | Routine fluid therapy |
| Rapid Infusion Set | Up to 48,000 mL/hr | Trauma and shock |
| RIC (Gravity) | 200–600 mL/min | High-flow peripheral access |
| RIC (Pressurized) | 1000–1200 mL/min | For rapid resuscitation |
| Single-Lumen CVC | ~125 mL/min | Central venous access |
| Multi-Lumen CVC | 26–52 mL/min | Lower flow per channel |
Which complications can happen from picking the wrong needle size?
Complications from picking the wrong needle size include infiltration, phlebitis, blockage, and extravasation. Overall peripheral IV failure rates range from 35-50%, with infiltration/blockage happening in 23% of cases (Marsh et al., 2021; AVA Standards, 2024). A 2022 study on catheter gauge selection revealed 26G catheters decrease phlebitis and blockage risk, while 24G catheters increase infiltration rates (Liu et al., 2022).
According to a 2010 study on contrast injection, 22G IV catheters show 2.2% extravasation rate, much higher than other sizes (Wienbeck et al., 2010). Local complications happen in over 50% of patients but often go unnoticed (Chaudhary et al., 2020). Infiltration with RICs can quickly cause compartment syndrome, especially with pressurized infusion (EMRA, 2025). These complications show why proper IV needle size selection stays critical for your safety and successful treatment results.
Which IV Needle Sizes Are Commonly Used in Medical Settings?
IV needle sizes commonly used in medical settings vary based on patient population, medical needs, and specific procedures. Standard adult care uses 20G-22G catheters for routine fluids and medications, while emergency situations need bigger gauges for rapid infusion. Kids need smaller gauges because of their delicate blood vessels, and specialty situations require specific catheter types beyond standard peripheral IVs.
What are the standard IV needle sizes for adults?
The standard IV needle sizes for adults are 20G-22G catheters for most hospitalized patients needing IV fluids and medications. According to Lippincott NursingCenter 2025, these gauges balance flow rates with your comfort. Blood transfusions need 18G-20G catheters to prevent blood cell damage and ensure good flow.
Emergency trauma patients need 14G-16G catheters for rapid infusion of fluids and blood. Radiology departments prefer 20G or bigger for CT and MRI studies with IV contrast. Surgical society guidelines recommend two 18-gauge or bigger peripheral IVs for critically injured trauma patients, as reported by EMRA in 2025.
What sizes are generally used for kids?
The sizes generally used for kids are 24G catheters for peripheral IV placement in pediatric emergency departments. CHOP Guidelines 2025 establish 24G as the traditional standard. Newborns need 26-24G peripheral IV catheters, with 27-25G for head needles according to DeltaMed 2021. Starship Hospital’s 2021 protocols specify Terumo Surflow 24G and 22G radiopaque Teflon catheters as current standards in newborn services.
A 2019 study by Choden et al. found pediatric first-try IV success rate at 64%, much lower than adult populations. Multiple studies from 2020-2024 show ultrasound guidance improves pediatric first-try success rates, often exceeding 85%.

When are specialty sizes or catheters preferred?
Specialty sizes or catheters are preferred when standard peripheral access can’t meet medical requirements. Vasopressors infuse safely through 16G-18G peripheral IVs for up to 24 hours before needing central access, per Lippincott NursingCenter 2025. PICC lines serve long-term IV therapy, TPN, antibiotics, and chemotherapy when peripheral access proves inadequate.
A 2020 study by Tsuji et al. found midline catheters measuring 8-20 cm benefit obese patients with difficult venous access. Extended Dwell Peripheral IV devices support longer stays for newborns with difficult vascular access, according to the 2018 Reducing Venous Depletion report. These specialty devices bridge the gap between standard peripheral IVs and central venous catheters, providing in-between solutions for complex vascular access needs.
How Do Healthcare Providers Decide Which IV Needle Size to Use?
Healthcare providers pick IV needle sizes through careful assessment of your characteristics, medication requirements, and vein conditions. The A-DIVA scale predicts difficult IV access using five factors: history of difficult access (OR 2.7), expected difficulty (OR 2.6), inability to feel vein (OR 4.8), inability to see vein (OR 5.9), and vein width less than 3mm (OR 3.5) according to a 2019 study by van Loon et al. These factors guide providers toward the right gauge selection before they try to insert.
What patient factors influence IV needle size choice?
Patient factors influencing IV needle size choice include age, gender, medical history, and body composition. A 2021 study by Marsh et al. found that female patients experience higher complication rates with phlebitis (HR 1.98) and infiltration/blockage (HR 1.45) compared to males. Patients aged 50 years and older show 1.4% extravasation rate versus 0.6% in younger patients during contrast injection according to 2010 research by Wienbeck et al.
Predictive factors for difficult access include obesity, chronic illness, low blood volume, IV drug abuse history, blood vessel disease, and swelling. Each year increase in age provides slight protection against complications with HR 0.99 for both phlebitis and all-cause failure. These patient-specific factors require providers to balance catheter stability with vein preservation when picking needle gauges.
How do the type of fluids or medications impact needle size selection?
The type of fluids or medications directly determines minimum acceptable catheter gauge requirements. Blood transfusions need 18G-20G catheters to prevent blood cell damage and ensure good flow. Intravenous antibiotics present the strongest provider risk factor for infiltration/blockage (HR 1.40) and phlebitis (HR 1.36) based on 2021 data from Marsh et al.
Vesicant chemotherapy agents need careful size selection because of severe tissue injury risk from extravasation. A 2022 study by Liu et al. showed that irritant drug infusion increases phlebitis and infiltration rates regardless of catheter size. Rapid Infusion Catheters are not intended for high-dose vasopressors or vesicants as they provide peripheral, not central access.
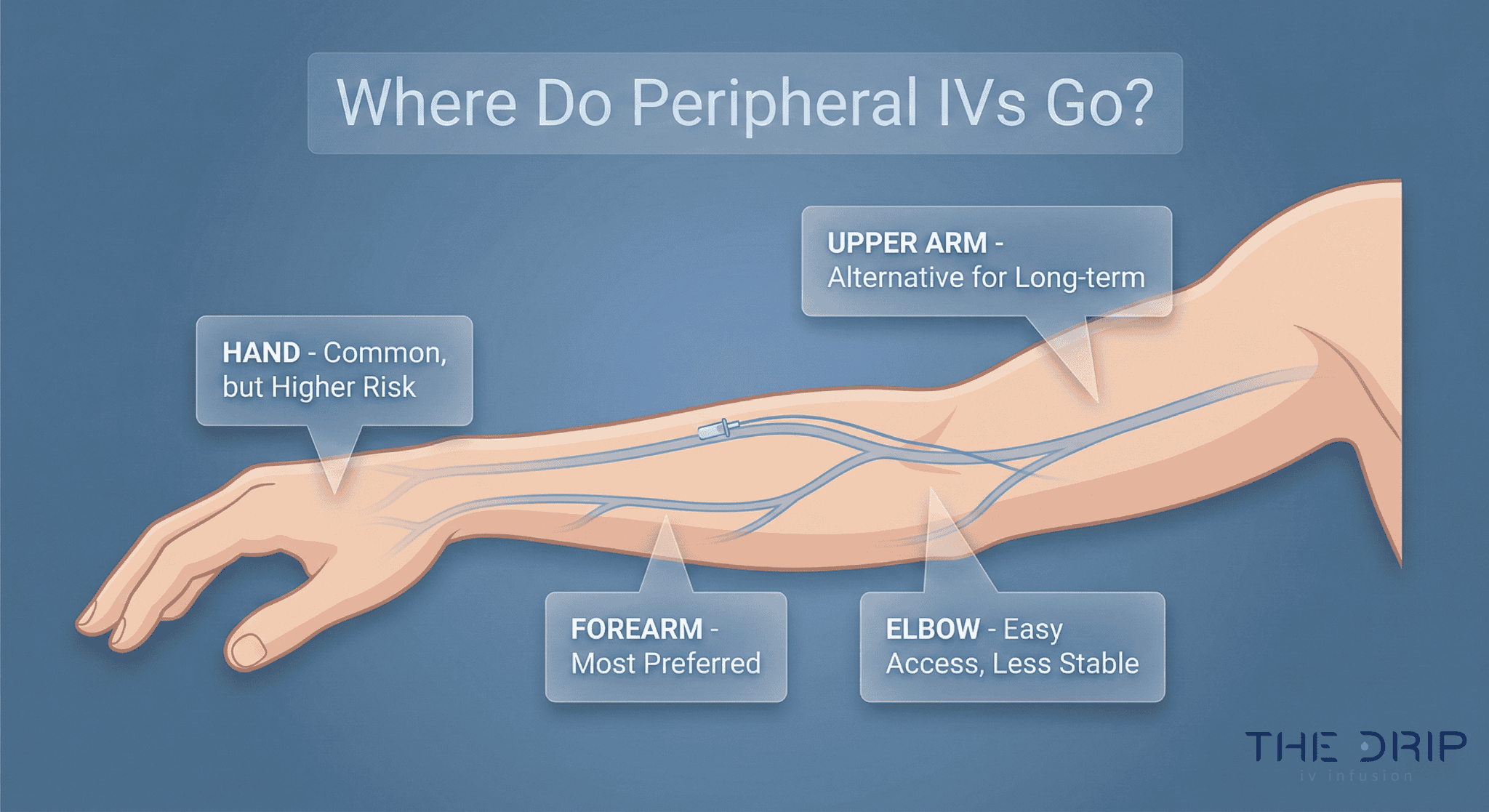
How does vein condition affect IV needle sizing?
Vein condition guides needle sizing through several predictable factors. Providers typically check for:
- Vein width under 3 mm
- Vein fragility or rolling (common in elderly patients)
- Wrist or hand insertion site
- Antecubital fossa positioning
- Back-of-hand fragility and blockage risk
How Do IV Needle Sizes Compare to Each Other and to Other Devices?
IV needle sizes follow different measurement systems depending on device type. Peripheral IV catheters use gauge sizing from 14G to 24G, while central venous catheters use French sizing where 8 French equals 2.8mm according to Lippincott NursingCenter 2025. Understanding these differences helps doctors and nurses pick the right devices for specific medical needs.
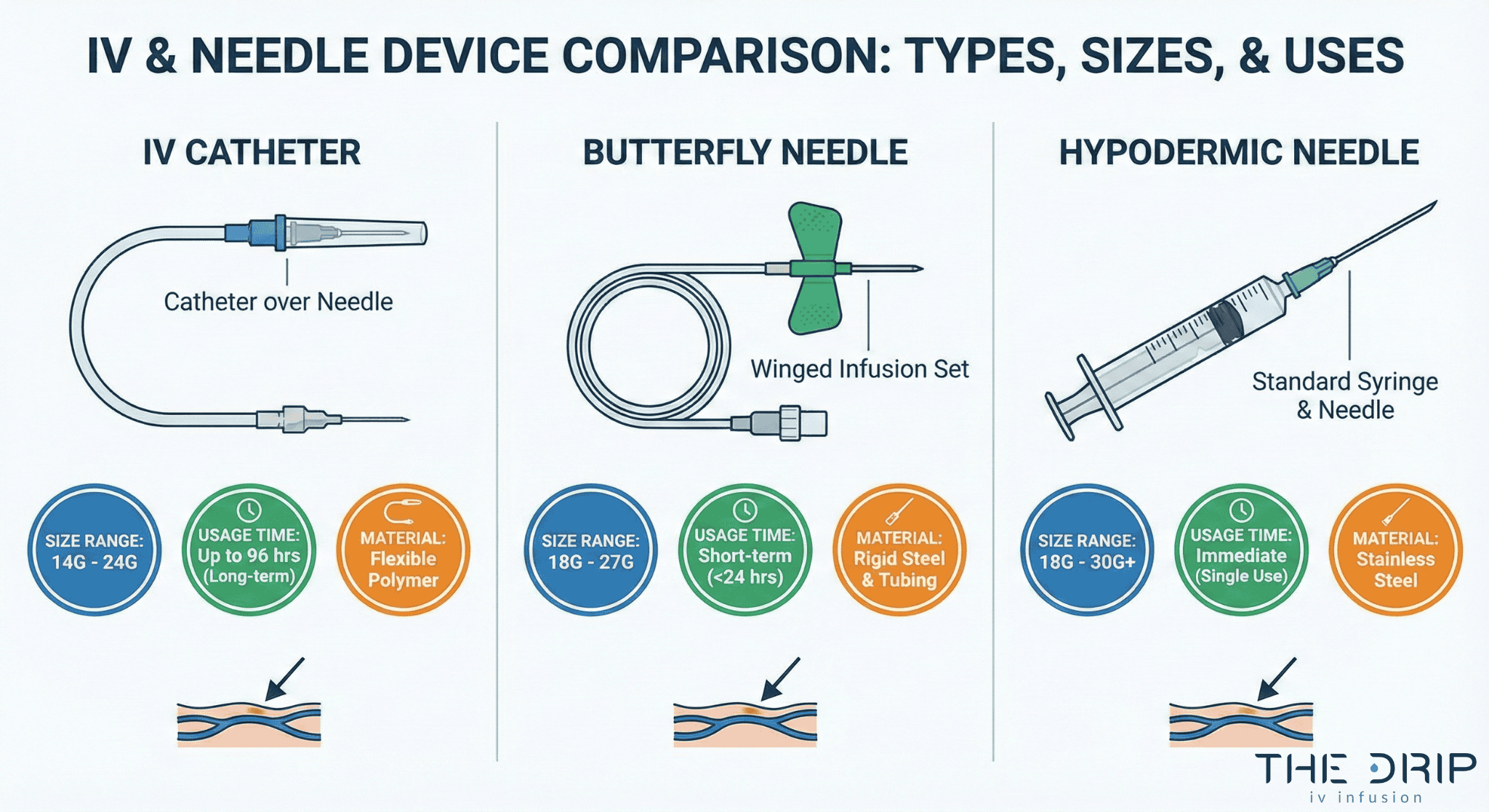
How do IV needle gauges differ from butterfly needles?
Butterfly needles differ from standard IV catheters in construction and use. Butterfly needles have wings for stabilization during short-term use, while IV catheters have plastic tubes that stay in place after needle removal.
Standard butterfly needles range from 18G to 27G with shorter lengths of 0.5 to 0.75 inches. IV catheters provide longer stay times up to 96 hours compared to butterfly needles designed for immediate use. Flow rates vary a lot between devices based on gauge and length specifications.
What are the similarities and differences between IV catheters and hypodermic needles?
IV catheters and hypodermic needles share gauge sizing but differ fundamentally in design and function. Both use the same gauge measurement system where smaller numbers mean bigger widths. Hypodermic needles consist entirely of metal for single-use injection or withdrawal. IV catheters combine a metal introducer needle with a plastic tube that stays in the vein.
Material differences affect performance a lot. BD Vialon catheters and B. Braun polyurethane catheters offer different properties affecting insertion success and stay time according to 2025 manufacturer specifications. Smiths Medical Jelco catheters use FEP polymer construction with “J”-point needle design for improved vein entry feel per Smiths Medical 2025 data.
Flow rate capabilities distinguish these devices clearly. A 14G peripheral catheter delivers 240 mL/min while an 8Fr introducer achieves up to 300 mL/min according to Lippincott NursingCenter 2025. These differences determine the right uses for rapid resuscitation versus routine medication administration.
How do compatibility and use cases vary with different devices?
Device compatibility depends on medical requirements and patient factors. BD Instaflash Needle Technology with notched needle design spans 18-24 gauge sizes for improved first-stick success according to BD 2025. Infusion tubing selection affects overall flow capacity with standard sets limiting flow to 12,000 ml/hr while rapid sets allow 48,000 ml/hr per Lippincott NursingCenter 2025.
Specialized equipment enhances success rates in challenging cases. A 2019 study by Choden et al. showed that transilluminator use achieved 82% eventual successful placement in 52 pediatric patients with difficult access. Safety considerations require FDA-cleared sharps disposal containers classified as class II devices requiring 510(k) premarket notification according to FDA 2021 regulations.
Selection criteria vary by patient population and therapy type. Kids benefit from smaller gauges with visualization aids. Emergency settings need bigger bore access for rapid resuscitation. Long-term therapy needs durable materials with lower infection risks. The next section explores best practices for inserting and handling these various needle sizes safely and effectively.
What Are Best Practices for Inserting and Handling IV Needles of Various Sizes?
Best practices for inserting and handling IV needles require understanding proper technique, complication prevention, and safety protocols. The 2024 INS Standards recommend picking the smallest outer width with fewest channels that stays least invasive for prescribed therapy. Following evidence-based guidelines ensures optimal patient outcomes across all needle sizes.
What are the recommended techniques for inserting different needle sizes?
The recommended techniques for inserting different needle sizes begin with picking the smallest appropriate catheter width. According to the 2024 INS Standards, doctors and nurses should choose the smallest outer width with fewest channels that is least invasive for prescribed therapy. B. Braun’s Universal Bevel geometry allows wider insertion angle choices to adapt to various clinical situations.
First-try success rates in adults average 81% using standard techniques, according to a 2019 study by van Loon et al. Ultrasound guidance improves success rates for difficult access patients, particularly those with high DIVA scores, as shown in D’Alessandro et al.’s 2023 research. A 2019 study by Choden et al. found that lighter skin color, visible vein with tourniquet, and left hand use predict successful first-try insertion.
Key insertion factors include:
- Patient positioning with arm below heart level
- Tourniquet application 4-6 inches above site
- Skin cleaning with appropriate drying time
- Insertion angle of 10-30 degrees depending on vein depth
- Blood flashback confirmation before advancing catheter
These standard techniques apply across gauge sizes while adapting angle and approach based on vein characteristics.
How can doctors and nurses minimize complications related to needle size?
Doctors and nurses can minimize complications related to needle size through proper patient selection and maintenance protocols. A 2022 study by Liu et al. found catheters left in for over 96 hours show no higher complication rate with medically-indicated replacement versus routine replacement. The same research identified surgical department patients as having increased susceptibility to infiltration, phlebitis, and blockage.
Using needleless connectors reduces blockage risk compared to non-use, according to Liu et al.’s 2022 findings. The 2024 AVA Standards emphasize that PIVC insertion and maintenance stays underappreciated with fundamental lack of awareness regarding associated risks. The NCBI Nursing Advanced Skills guide (2025) recommends avoiding rapid infusion into fragile veins to prevent complications in elderly patients.
| Entity | Attribute | Value | Source/Year |
| Catheter dwell time | Complication threshold | >96 hours no increase | Liu 2022 |
| Surgical patients | Risk elevation | Higher infiltration/phlebitis | Liu 2022 |
| Needleless connectors | Occlusion reduction | Significant decrease | Liu 2022 |
| Elderly veins | Infusion rate | Slower required | NCBI 2025 |
Regular assessment and early intervention prevent minor issues from becoming serious complications.
What safety measures should be followed for disposal and handling?
Safety measures for disposal and handling follow strict regulatory requirements. Sharps disposal requires strict adherence to safety steps:
- Activate catheter safety mechanism immediately after removal
- Place the used device directly into an approved sharps container
- Never recap used needles
- Keep containers below the fill line
- Replace containers when ¾ full
| Regulatory Body | Requirement | Description |
| OSHA | Safety mechanisms | Required under Bloodborne Pathogens Standard |
| FDA | Sharps container approval | Must be 510(k)-cleared puncture-resistant containers |
| CDC | Proper container usage | No recapping; place at point of use |
| WHO | Global PIVC handling guidance | Standardized insertion/maintenance/removal |
These comprehensive best practices ensure safe, effective IV therapy delivery while minimizing risks to both patients and healthcare workers across all clinical settings.
How Should You Approach IV Needle Size Selection and Care with The Drip IV Infusion?
IV needle size selection needs medical expertise and patient-specific assessment. The Drip IV Infusion follows evidence-based protocols for catheter selection, prioritizing your comfort while ensuring therapeutic effectiveness. Professional providers evaluate multiple factors including vein condition, treatment type, and individual anatomy before picking appropriate gauge sizes.
The following subsections detail how The Drip IV Infusion approaches needle selection and the critical factors governing IV catheter choices in medical practice.
Can The Drip IV Infusion help you choose the right IV needle size for your needs?
The Drip IV Infusion helps you choose the right IV needle size through professional assessment and standard protocols. The global peripheral IV catheter market valued at $5.4 billion in 2023 reflects widespread medical reliance on proper catheter selection (GM Insights, 2023). Healthcare providers use over 2 billion catheters annually worldwide, with the US purchasing 330 million PIVCs yearly (AVA Standards, 2024).
Professional IV therapy services use products from major manufacturers including Becton Dickinson, Teleflex, ICU Medical, and B. Braun (Markets and Markets, 2025). Medical data shows 81% of emergency department patients receive PIVCs, though 49% remain unused during admission (Willis et al., 2024). The Drip IV Infusion’s trained professionals assess each patient’s needs, vein condition, and therapy requirements to pick optimal catheter sizes.
Proper gauge selection minimizes complications while ensuring effective treatment delivery. The service follows industry best practices for catheter insertion and maintenance, reducing failure risks through appropriate sizing decisions.
What are the key takeaways about IV needle sizes discussed above?
To ensure safe, comfortable, and effective treatment, proper IV needle sizes must be selected based on vein condition, therapy type, and individual assessment. By following evidence-based standards from AVA, INS, AACN, and ECRI, The Drip IV Infusion ensures that every patient receives the most appropriate catheter choice. If you’re preparing for infusion therapy, understanding IV needle sizes helps you ask better questions and feel more confident in your care.